Archive for the ‘MERS-CoV’ Category
Saudi Arabia has now reported 153 MERS-CoV cases for this year.
Tuesday, June 25th, 2019Health Events: Epi-week 25, 2019 م2019 ﻌﻟﺎم 25 ثاﺪﺣأ اﻷﺳﺒﻮع اﻟﻮﺑﺎﺋﻲ
Date ﺦﻳرﺎﺘﻟا
Event# ﻢﻗر ثﺪﺤﻟا
Description
اﻟﻮﺻﻒ
20/06/2019 19-1931
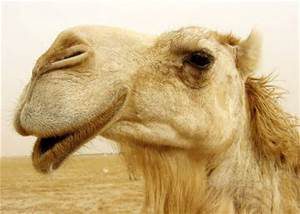
MERS from Madinah City: a 70-year-old male in Madinah city, Madinah region Contact with camels: Yes Case classification: Primary Current status: Active
ﻣ ﺔﻣزﻼﺘ قﺮﺸﻟا ﻂﺳوﻷا ﺔﻴﺴﻔﻨﺘﻟا ﻦﻣ ﺔﻨﻳﺪﻣ اﻟﻤﺪﻳﺔﻨ اﻟﻤﻨﻮرة: ﻣﻨﻄﻘﺔ ، ﻋﺎ ًﻣﺎ ﻦﻣ ﺔﻨﻳﺪﻣ اﻟﻤﺪﻳﻨﺔ اﻟ ةرﻮﻨﻤ 70 ﻞﺟر ﺒﻳﻎﻠ اﻟﻤﺪﻳﻨﺔ اﻟﻤﻨﻮرة ﺔﻄﻟﺎﺨﻣ ﻞﺑﻺﻟ :ﻢﻌﻧ ﻒﻴﻨﺼﺗ ﺔﻟﺎﺤﻟا :ﺔﻴﻟوأ ﺔﻟﺎﺣ اﻟﻤﺮﻳﺾ :ﺔﻄﺸﻧ
22/06/2019 19-1932
MERS from AlRass City: a 42-year-old male in AlRass city, Qassim region Contact with camels: Yes Case classification: Primary Current status: Active
ﻣ ﺔﻣزﻼﺘ قﺮﺸﻟا ﻂﺳوﻷا ﺔﻴﺴﻔﻨﺘﻟا ﻦﻣ ﺔﻨﻳﺪﻣ ﻟاسﺮ: ﻣﻨﻄﻘﺔ اﻟﻘﺼﻴﻢ ، ﻋﺎ ًﻣﺎ ﻦﻣ ﺔﻨﻳﺪﻣ اﻟﺮس 42 ﻞﺟر ﺒﻳﻎﻠ ﺔﻄﻟﺎﺨﻣ ﻞﺑﻺﻟ :ﻢﻌﻧ ﻒﻴﻨﺼﺗ ﺔﻟﺎﺤﻟا :ﺔﻴﻟوأ ﺔﻟﺎﺣ اﻟﻤﺮﻳﺾ :ﺔﻄﺸﻧ
A MERS-CoV outbreak in Wadi ad-Dawasir, Saudi Arabia: Since January, officials have identified 61 cases in the city, of which 14 were in health workers, and 37 were thought to involve healthcare exposure.
Saturday, April 27th, 2019Middle East respiratory syndrome coronavirus (MERS-CoV) – The Kingdom of Saudi Arabia
From 14 February through 31 March 2019, the National IHR Focal Point of Saudi Arabia reported 22 additional cases of Middle East respiratory syndrome coronavirus (MERS-CoV) infection, including four deaths, associated with the outbreak in Wadi Aldwasir. Of the 22 cases, 19 were reported from Wadi Aldwasir city including two healthcare workers. The remaining three cases, which are epidemiologically linked to the outbreak, were healthcare workers from a hospital in Khamees Mushait city, Asir region.

Since the beginning of this outbreak in January 2019, a total of 61 MERS-CoV cases, with a case fatality ratio of 13.1% (8/61), have been reported in Wadi Aldwasir city. The median age of reported cases was 46 years (range 16 to 85 years). Of the 61 cases, 65% (n=46) were male, and 23% (n = 14) were health care workers. Investigations into the source of infection of the 61 cases found that 37 were health-care acquired infections, 14 were primary cases presumed to be infected from contact with dromedary camels and the remaining (10) infections occurred among close contacts outside of health care settings. As previously reported1, two human to human transmission amplification events took place at a hospital during this outbreak (one amplification event in the emergency department, and one amplification event in a cardiac intensive care unit; Figure 1).
The link below provides details of the 22 reported cases:
From 2012 through 31 March 2019, a total of 2399 laboratory-confirmed cases of MERS-CoV and 827 associated deaths were reported globally to WHO under the International Health Regulations (IHR). The associated deaths reported to WHO were identified through follow-up with affected member states.
Public Health Response
As reported previously, the Saudi Arabian Ministry of Health (MoH) has conducted and completed a full-scale investigation of the MERS outbreak in Wadi Aldwasir including identification of all household and healthcare worker contacts of confirmed patients in all of the hospitals affected.
As of 31 March 2019, a total of 380 contacts have been identified, including 260 household contacts and 120 healthcare worker contacts. All identified contacts were monitored for 14 days from the last date of exposure as per WHO and national guidelines for MERS. All secondary cases have been reported to WHO.
Currently, all the listed contacts have been tested for MERS-CoV infection by reverse transcription polymerase chain reaction (RT-PCR) at least once and many contacts of known patients have been tested repeatedly. All secondary cases of MERS-CoV infection have been reported to WHO. The last case from Wadi Aldwasir was reported on 12 March 2019.
Within the affected health care facilities, infection prevention and control measures have been enhanced including intensive mandatory on-the-job training on infection control measures for all healthcare workers in emergency room and intensive care unit. Disinfection has been carried out in the emergency room and ICU of hospital A, which is fully operational and additional staff were mobilized to support infection control activities. Respiratory triage has been enforced in all healthcare facilities in the Riyadh region.
The MoH media department launched an awareness campaign targeting Wadi Aldawasir city with special focus on camel owners and camel related activities.
The Ministry of Agriculture is testing dromedaries in Wadi Aldwasir city and initial results have identified several PCR positive dromedaries in the city. Positive camels have been removed from the market and movement in and out of the camel market has been restricted. Camels owned by confirmed human cases were quarantined regardless of testing results. Full genome sequencing of available human and dromedary specimens have been conducted. Laboratory findings of camel testing by the Ministry of Agriculture have been reported to the World Organization for Animal Health (OIE).
WHO risk assessment
Infection with MERS-CoV can cause severe disease resulting in high morbidity and mortality. Humans are infected with MERS-CoV from direct or indirect contact with infected dromedary camels or by transmission between humans. So far, the observed non-sustained human-to-human transmission has occurred mainly in health care settings.
The notification of these additional cases does not change WHO’s overall risk assessment of MERS. WHO expects that additional cases of MERS will be reported from the Middle East, and that cases will continue to be exported to other countries by individuals who might acquire the infection after exposure to dromedary camels, dromedary camel animal products (for example, consumption of camel’s raw milk), or humans (for example, in a health care setting or household contacts).
WHO continues to monitor the epidemiological situation and conducts risk assessment based on the latest available information. Results of the completed epidemiological investigation, as well as full genome sequencing of available dromedary and human specimens are being used by Ministry of Health officials to further evaluate the zoonotic and human-to-human transmission that has occurred in Wadi Aldwasir outbreak.
WHO advice
Based on the current situation and available information, WHO encourages all Member States to continue their surveillance for acute respiratory infections and to carefully review any unusual patterns.
Infection prevention and control (IPC) measures are critical to prevent the possible spread of MERS-CoV in health care facilities. It is not always possible to identify patients with MERS-CoV infection early because like other respiratory infections, the early symptoms of MERS are non-specific. Therefore, healthcare workers should always apply standard precautions consistently with all patients, regardless of their diagnosis. Droplet precautions should be added to the standard precautions when providing care to patients with symptoms of acute respiratory infection; contact precautions and eye protection should be added when caring for probable or confirmed cases of MERS; airborne precautions should be applied when performing aerosol generating procedures.
Early identification, case management and isolation, together with appropriate infection prevention and control measures can prevent human-to-human transmission of MERS-CoV.
WHO recommends that comprehensive identification, follow up and testing of all contacts of MERS patients be conducted, if feasible, regardless of the development of symptoms since approximately 20% of all reported MERS cases have been reported as mild or asymptomatic. The role of asymptomatic MERS-CoV infection in transmission is not well understood. However, reports of transmission from an asymptomatic MERS patient to another individual have been documented.
MERS causes more severe disease in people with underlying chronic medical conditions such as diabetes mellitus, renal failure, chronic lung disease, and compromised immune systems. Therefore, people with these underlying medical conditions should avoid close unprotected contact with animals, particularly dromedary camels, when visiting farms, markets, or barn areas where the virus is known to be potentially circulating. General hygiene measures, such as regular hand washing before and after touching animals and avoiding contact with sick animals, should be adhered to.
Food hygiene practices should be observed. People should avoid drinking camel’s raw milk or camel urine or eating camel meat that has not been properly cooked.
WHO does not advise special screening at points of entry with regard to this event nor does it currently recommend the application of any travel or trade restrictions.
Saudi Arabia’s MERS-CoV total for the year comes to 134 cases
Tuesday, April 23rd, 201922/04/2019 19-1911
MERS in Madinah city: 56-year-old male in Madinah city, Madinah region
Contact with camels: Unknown
Case classification: Primary
Current status: Active
Saudi MERS: 107 cases for 2019, including 57 linked to a large outbreak in Wadi ad-Dawasir in which most cases were linked to healthcare exposure.
Tuesday, April 2nd, 2019Health Events: Epi-week 13, 2019 132019
Date التاريخ
Event# رقم الحدث
Description
الوصف
25/03/2019 19-1883
MERS in Khamees Meshait city: 61-year-old male in Khamess Meshait city, Aseer region Contact with camels: No Case classification: Primary Current status: Active
61
27/03/2019 19-1884
MERS in Alkharj city: 57-year-old male in Alkharj city, Riyadh region Contact with camels: Yes Case classification: Primary Current status: Active
57
27/03/2019 19-1885
MERS in Hufoof city: 60-year-old female in Hufoof city, Alhsa region Contact with camels: No Case classification: Primary Current status: Active
Saudi Arabia: From 1 through 28 February 2019, 68 additional cases of Middle East respiratory syndrome coronavirus (MERS-CoV) infection, including 10 deaths.
Saturday, March 30th, 2019This Disease Outbreak News update describes the 19 cases. Among these cases, fifteen were sporadic, and four were reported as part of two unrelated clusters. Cluster 1 involved two cases in Buridah city; and Cluster 2 involved two cases in Riyadh city. The link below provides details of the 19 reported cases.
A separate Disease Outbreak News will provide an update on the outbreak in Wadi Aldwasir which affected 49 cases and resulted in seven deaths in February making a total of 52 cases since the onset of the outbreak.
From 2012 through 28 February 2019, the total number of laboratory-confirmed MERS cases reported globally to WHO is 2374 with 823 associated deaths. The global number reflects the total number of laboratory-confirmed cases reported to WHO under IHR to date. The total number of deaths includes the deaths that WHO is aware of to date through follow-up with affected member states.
WHO risk assessment
Infection with MERS-CoV can cause severe disease resulting in high morbidity and mortality. Humans are infected with MERS-CoV from direct or indirect contact with infected dromedary camels. MERS-CoV has demonstrated the ability to transmit between humans, especially from close unprotected contact with infected patients. So far, the observed non-sustained human-to-human transmission has occurred mainly in health care settings.
The notification of these additional cases does not change WHO’s overall risk assessment of MERS. WHO expects that additional cases of MERS will be reported from the Middle East, and that cases will continue to be exported to other countries by individuals who might acquire the infection after exposure to dromedary camels, animal products (e.g. consumption of camel’s raw milk), or humans (e.g. in a health care setting). WHO continues to monitor the epidemiological situation and conducts risk assessment based on the latest available information.
WHO advice
Based on the current situation and available information, WHO encourages all Member States to continue their surveillance for acute respiratory infections and to carefully review any unusual patterns.
Infection prevention and control (IPC) measures are critical to prevent the possible spread of MERS-CoV in health care facilities. It is not always possible to identify patients with MERS-CoV infection early because like other respiratory infections, the early symptoms of MERS are non-specific. Therefore, healthcare workers should always apply standard precautions consistently with all patients, regardless of their diagnosis. Droplet precautions should be added to the standard precautions when providing care to patients with symptoms of acute respiratory infection; contact precautions and eye protection should be added when caring for probable or confirmed cases of MERS; airborne precautions should be applied when performing aerosol generating procedures.
Early identification, case management and isolation, together with appropriate infection prevention and control measures can prevent human-to-human transmission of MERS-CoV.
WHO recommends that comprehensive identification, follow up and testing of all contacts of MERS patients be conducted, if feasible, regardless of the development of symptoms since approximately 20% of all reported MERS cases have been reported as mild or asymptomatic. The role of asymptomatic MERS-CoV infection in transmission is not well understood. However, reports of transmission from an asymptomatic MERS patient to another individual have been documented.
MERS causes more severe disease in people with underlying chronic medical conditions such as diabetes mellitus, renal failure, chronic lung disease, and compromised immune systems. Therefore, people with these underlying medical conditions should avoid close unprotected contact with animals, particularly dromedary camels, when visiting farms, markets, or barn areas where the virus is known to be potentially circulating. General hygiene measures, such as regular hand washing before and after touching animals and avoiding contact with sick animals, should be adhered to.
Food hygiene practices should be observed. People should avoid drinking camel’s raw milk or camel urine or eating camel meat that has not been properly cooked.
WHO does not advise special screening at points of entry with regard to this event nor does it currently recommend the application of any travel or trade restrictions.
A review: Dromedary camels as the main reservoir for human Middle East respiratory syndrome (MERS) infections.
Saturday, March 16th, 2019Sikkema, R., Farag, E., Islam, M., Atta, M., Reusken, C., Al-Hajri, M., & Koopmans, M. (2019). Global status of Middle East respiratory syndrome coronavirus in dromedary camels: A systematic review. Epidemiology and Infection, 147, E84. doi:10.1017/S095026881800345X
“…..In general, camels only show minor clinical signs of disease after being infected with MERS-CoV. Serological evidence of MERS-CoV in camels has been found in 20 countries, with molecular evidence for virus circulation in 13 countries. The seroprevalence of MERS-CoV antibodies increases with age in camels, while the prevalence of viral shedding as determined by MERS-CoV RNA detection in nasal swabs decreases. In several studies, camels that were sampled at animal markets or quarantine facilities were seropositive more often than camels at farms as well as imported camels vs. locally bred camels. Some studies show a relatively higher seroprevalence and viral detection during the cooler winter months. …..”
Saudi Arabia: 102 cases since the first of the year, of which 57 are linked to the outbreak in Wadi ad-Dawasir, most of which are linked to healthcare exposure, with some related to contact with camels.
Wednesday, March 13th, 2019Health Events: Epi-week 11, 2019 112019
Date التاريخ
Event# رقم الحدث
Description
الوصف
10/03/2019 19-1874
MERS in Hafr Albatin city: 47-year-old male in Hafr Albatin city, Hafr Albatin region Contact with camels: Yes Case classification: Secondary Current status: Active
47
10/03/2019 19-1875
MERS in Khamees Meshait city: 64-year-old female in Khamees Meshait city, Aseer region Contact with camels: No Case classification: Secondary Current status: Active
64
11/03/2019 19-1876
MERS in Wadi Aldwasir city: 60-year-old male in Wadi Aldwasir city, Riyadh region Contact with camels: No Case classification: Secondary Current status: Active
MERS-CoV in Oman: 8 new cases
Tuesday, March 5th, 2019Between 12 and 18 February 2019, the National IHR Focal Point of Oman reported eight additional cases of Middle East respiratory syndrome coronavirus (MERS-CoV) infection. Four cases were reported from South Sharquia governorate, and four cases were reported from North Batinah governorate where a MERS-CoV cluster was recently identified. Details of the additional eight cases can be found in the attached excel sheet.
Since 27 January 2019, a total of 13 MERS cases were reported from Oman, including nine from North Batinah (five cases were previously reported in the Disease outbreak News 11 February 2019) and four from South Sharquia.
An investigation into the exposure history to known risk factors in the 14 days prior to symptom onset in all eight cases is currently ongoing.
From 2012 through 18 February 2019, a total of 2357 laboratory-confirmed cases of MERS, along with 820 associated deaths, have been reported to WHO globally. The first reported MERS infection in Oman was reported in 2013. Since then, a total of 24 cases and seven deaths have been reported.
The global number reflects the total number of laboratory-confirmed cases reported to WHO under IHR to date. The total number of deaths includes the deaths that WHO is aware of to date through follow-up with affected member states.
Public Health response
Whole genome sequencing of available human specimens of patients is being conducted. As of 21 February, all identified contacts (family and health workers) of confirmed MERS patients have been screened, including 69 contacts from North Batinah patients and 57 contacts from South Sharqiyah patients. Tracing and follow-up of these contacts is ongoing by the Ministry of Health for 14 days from the last date of exposure as per WHO and national guidelines for MERS-CoV. All contacts have been sampled and have tested negative for MERS-CoV by RT-PCR.
The Ministry of Agriculture has conducted an investigation of dromedaries at the farms of one of the patients. Results of this investigation are pending.
The Ministry of Health has strengthened infection prevention and control measures in emergency departments, especially in triaging areas. Health education and awareness materials were produced and disseminated to health care staff, patients and visitors.
Family members of MERS-CoV infected patients have been contacted and advised about the virus and on measures to ensure personal protection to prevent infection. Efforts in improving public health awareness among the general public has been strengthened through greater messaging in the media.
WHO risk assessment
Infection with MERS-CoV can cause severe disease resulting in high morbidity and mortality. Humans are infected with MERS-CoV from direct or indirect contact with infected dromedary camels. MERS-CoV has demonstrated the ability to transmit between humans, especially from close unprotected contact with infected patients. So far, the observed non-sustained human-to-human transmission has occurred mainly in health care settings.
The notification of these additional cases does not change WHO’s overall risk assessment of MERS-CoV. WHO expects that additional cases of MERS infection will be reported from the Middle East, and that cases will continue to be exported to other countries by individuals who might acquire the infection after exposure to dromedary camels, animal products (e.g. consumption of camel’s raw milk), or humans (e.g. in a health care setting). WHO continues to monitor the epidemiological situation and conducts risk assessment based on the latest available information.
WHO advice
Based on the current situation and available information, WHO encourages all Member States to continue their surveillance for acute respiratory infections and to carefully review any unusual patterns.
Infection prevention and control measures are critical to prevent the possible spread of MERS-CoV between people in health care facilities. It is not always possible to identify patients with MERS-CoV infection early because like other respiratory infections, the early symptoms of MERS are non-specific. Therefore, healthcare workers should always apply standard precautions consistently with all patients, regardless of their diagnosis. Droplet precautions should be added to the standard precautions when providing care to patients with symptoms of acute respiratory infection; contact precautions and eye protection should be added when caring for probable or confirmed cases of MERS infection; airborne precautions should be applied when performing aerosol generating procedures.
Early identification, case management and isolation, together with appropriate infection prevention and control measures can prevent human-to-human transmission of MERS-CoV.
WHO recommends that comprehensive identification, follow up and testing of all contacts of MERS patients be conducted, if feasible, regardless of the development of symptoms since approximately 20% of all reported MERS infections have been reported as mild or asymptomatic. The role of asymptomatic MERS infection in transmission is not well understood. However, reports of transmission from an asymptomatic MERS infected patient to another individual have been documented.
MERS causes more severe disease in people with underlying chronic medical conditions such as diabetes, renal failure, chronic lung disease, and immunocompromised persons. Therefore, these people should avoid close contact with dromedary camels when visiting farms, markets, or barn areas where the virus is known to be potentially circulating. General hygiene measures, such as regular hand washing before and after touching animals and avoiding contact with sick animals, should be adhered to.
Food hygiene practices should be observed. People should avoid drinking raw camel milk or camel urine, and refrain from eating meat that has not been properly cooked.
WHO does not advise special screening at points of entry with regards to this event, and does not currently recommend the application of any travel or trade restrictions at this time.
The Saudi MOH has now confirmed 65 MERS infections since Jan 1
Tuesday, February 19th, 201918/02/2019 19-1841
MERS in Wadi Aldwasir city: 53-year-old male in Wadi Aldwasir city, Riyadh region
Contact with camels: Yes
Case classification: Primary
Current status: Hospitalized
Another MERS case in Saudi Arabia, making it 62 for the year
Monday, February 18th, 2019Middle East respiratory syndrome coronavirus (MERS-CoV) – Saudi Arabia
From 1 January through 31 January 2019, the International Health Regulations (IHR) National Focal Point of Saudi Arabia reported fourteen additional cases of Middle East respiratory syndrome coronavirus (MERS-CoV) infection, including three deaths. Details of these cases can be found by following the link to a separate document after this paragraph. Of the 14 cases reported in January, eight are from three separate clusters of cases. Cluster 1 involves three cases (listed as cases 1, 2 and 3) in Riyadh Province and cluster 2 involves two cases (listed as cases 4 and 5) in the city of Jeddah. Cluster 3 involves three cases (listed as cases 11, 13 and 14) in the city of Wadi Aldwaser and is currently ongoing. More details regarding the outbreak in Wadi Aldwaser and the implementation of interventions by the Ministry of Health (MoH) in Saudi Arabia will be provided in the next update.

The link below provides details of the fourteen reported additional cases.
From 2012 through 31 January 2019, the total number of laboratory-confirmed MERS-CoV cases reported globally to WHO under IHR (2005) is 2 298 with 811 associated deaths. The total number of deaths includes the deaths that WHO is aware of to date through follow-up with affected member states.
WHO risk assessment
Infection with MERS-CoV can cause severe disease resulting in high mortality. Humans are infected with MERS-CoV from direct or indirect contact with dromedary camels. MERS-CoV has demonstrated the ability to transmit between humans. So far, the observed non-sustained human-to-human transmission has occurred mainly in health care settings.
As of 15 February 2019, there is an ongoing outbreak of MERS in Wadi Aldwaser, which includes cases 11, 13 and 14 reported in the separate document linked above. WHO will provide details of the additional cases involved in this outbreak as well as intervention measures implemented by the MoH. The notification of additional cases does not change the overall risk assessment. WHO expects that additional cases of MERS-CoV infection will be reported from the Middle East, and that cases will continue to be exported to other countries by individuals who might acquire the infection after exposure to dromedary camels, animal products (for example, consumption of camel’s raw milk), or humans (for example, in a health care setting). WHO continues to monitor the epidemiological situation and conducts risk assessment based on the latest available information.
WHO advice
Based on the current situation and available information, WHO encourages all Member States to continue their surveillance for acute respiratory infections and to carefully review any unusual patterns.
Infection prevention and control measures are critical to prevent the possible spread of MERS-CoV in health care facilities. It is not always possible to identify patients with MERS-CoV early because like other respiratory infections, the early symptoms of MERS-CoV are non-specific. Therefore, healthcare workers should always apply standard precautions consistently with all patients, regardless of their diagnosis. Droplet precautions should be added to the standard precautions when providing care to patients with symptoms of acute respiratory infection; contact precautions and eye protection should be added when caring for probable or confirmed cases of MERS-CoV infection; airborne precautions should be applied when performing aerosol generating procedures. Early identification, case management and isolation, together with appropriate infection prevention and control measures can prevent human-to-human transmission of MERS-CoV.
MERS-CoV appears to cause more severe disease in people with diabetes, renal failure, chronic lung disease, and immunocompromised persons. Therefore, these people should avoid close contact with animals, particularly dromedary camels, when visiting farms, markets, or barn areas where the virus is known to be potentially circulating. General hygiene measures, such as regular hand washing before and after touching animals and avoiding contact with sick animals, should be adhered to. Food hygiene practices should be observed. People should avoid drinking raw camel milk or camel urine, or eating meat that has not been properly cooked.
WHO does not advise special screening at points of entry with regard to this event nor does it currently recommend the application of any travel or trade restrictions.