Salt Lake County Health Department
Archive for the ‘Zika virus’ Category
PAHO/WHO updates the characterization of Zika Congenital Syndrome
Tuesday, July 26th, 2016Washington, 22 July 2016 (PAHO/WHO) — The Pan American Health Organization/World Health Organization (PAHO/WHO) has updated its preliminary characterization of Zika Congenital Syndrome, after an international meeting in Pernambuco.
The event gathered scientists from Brazil, Colombia, Argentina, the United States, PAHO and WHO to investigate the details of Zika virus infection and its effects on the child. The update aims to contribute to improvement of the care provided in health services in the affected regions.
PAHO/WHO is leading a process to gather and review more evidence to clearly define these effects and will update its description as further evidence is produced.
In addition to previously known signs, such as microcephaly and some brain abnormalities described earlier, other aspects characterizing the Zika Congenital Syndrome have been identified.
They include clinical conditions and neuroimaging findings mainly related to the central nervous system such as epilepsy, hearing and visual impairment, and psychomotor development as well as effects on the bones and joints, or the osteoarticular system. These conditions have been characterized and analyzed in terms of frequency and severity in the time periods including antenatal, neonatal (0 to 28 days) and the child’s first year.
The scientists looked at systematic reviews of data on Zika, and shared country experiences from Brazil and Colombia. They heard an overview of the epidemiological situation, presented by PAHO’s Incident Manager for Zika, Dr. Sylvain Aldighieri, and visited health care facilities in Recife that care for infants who have microcephaly and other conditions associated with Zika virus infection.
The experts noted, “The range of abnormalities seen and the likely causal relationship with Zika virus infection suggest the presence of a new congenital syndrome. WHO has set in place a process for defining the spectrum of this syndrome. The process focuses on mapping and analyzing the clinical manifestations encompassing the neurological, hearing, visual and other abnormalities, and neuroimaging findings.”
Information on the complications resulting from Zika virus infection is still limited, and the scientists shared data on diagnosis, description, consequences, physical processes and analysis of evidence from clinicians and researchers on their main findings so far.
“Our aim is to assist the countries in strengthening surveillance of Zika and Zika Congenital Syndrome, in addition to enhancing readiness for dealing with Guillain-Barré cases in health services. The spatial and temporal association of Zika and Guillain-Barré syndrome is evident in various countries,” noted PAHO/WHO’s Aldighieri.
“We had the opportunity to go to IMIP (Instituto de Medicina Integral Professor Fernando Figueira), in Pernambuco, and see the excellent, incredible, work that they are doing in following up and taking care of about 200 children with microcephaly. It’s important that we get this kind of work to other parts of Brazil and the world for children affected with microcephaly,” said PAHO/WHO’s Director of Family, Gender and Life Course, Dr. Andres de Francisco. “We also should remember that Zika is not the only cause of microcephaly and microcephaly is not the only possible sign of Zika,” he added.
Dr. Luis Codina, PAHO/WHO’s deputy representative in Brazil, said, “After almost a year of very strong work done by various groups of researchers, today there is a certain consensus in associating Zika not only with microcephaly, but also with other aspects of a congenital syndrome. PAHO wants to facilitate this process of investigation and generation of knowledge.”
A team from Brazil’s Fiocruz Institute reported that Culex quinquefasciatus mosquitoes are a potential Zika virus vector.
Monday, July 25th, 2016
Culex quinquefasciatus
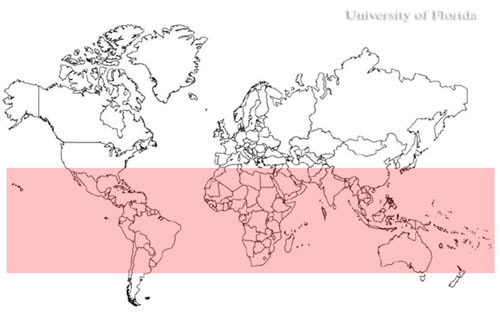
World distribution of the southern house mosquito, Culex quinquefasciatus
CDC: Pregnant Women with Any Laboratory Evidence of Possible Zika Virus Infection
Monday, July 25th, 2016Pregnant Women with Any Laboratory Evidence of Possible Zika Virus Infection in the United States and Territories, 2016
Pregnant Women with Any Laboratory Evidence of Possible Zika Virus Infection
US States and the District of Columbia*
400
*Includes aggregated data reported to the US Zika Pregnancy Registry as of July 14, 2016
US Territories**
378
**Includes aggregated data from the US territories reported to the US Zika Pregnancy Registry and data from Puerto Rico reported to the Zika Active Pregnancy Surveillance System as of July 14, 2016
About These Numbers
What these updated numbers show
- These updated numbers reflect counts of pregnant women in the United States with any laboratory evidence of possible Zika virus infection, with or without symptoms. Pregnant women with laboratory evidence include those in whom viral particles have been detected and those with evidence of an immune reaction to a recent virus that is likely to be Zika.
- This information will help healthcare providers as they counsel pregnant women affected by Zika and is essential for planning at the federal, state, and local levels for clinical, public health, and other services needed to support pregnant women and families affected by Zika.
What these new numbers do not show
- These new numbers are not comparable to the previous reports. These updated numbers reflect a different, broader population of pregnant women.
- These updated numbers are not real time estimates. They will reflect the number of pregnant women reported with any laboratory evidence of possible Zika virus infection as of 12 noon every Thursday the week prior; numbers will be delayed one week.
Where do these numbers come from?
These data reflect pregnant women in the US Zika Pregnancy Registry and the Zika Active Pregnancy Surveillance System in Puerto Rico. CDC, in collaboration with state, local, tribal and territorial health departments, established these registries for comprehensive monitoring of pregnancy and infant outcomes following Zika virus infection.
The data collected through these registries will be used to update recommendations for clinical care, to plan for services and support for pregnant women and families affected by Zika virus, and to improve prevention of Zika virus infection during pregnancy.
What are the outcomes for these pregnancies?
Visit CDC’s webpage for updated counts of poor pregnancy outcomes related to Zika. Most of the pregnancies monitored by these systems are ongoing. CDC will not report outcomes until pregnancies are complete.
Outcomes of Pregnancies with Laboratory Evidence of Possible Zika Virus Infection in the United States, 2016
Monday, July 25th, 2016Outcomes of Pregnancies with Laboratory Evidence of Possible Zika Virus Infection in the United States, 2016
Pregnancy Outcomes in the United States and the District of Columbia
Liveborn infants with birth defects*
12
Includes aggregated data reported to the US Zika Pregnancy Registry as of July 14, 2016
Pregnancy losses with birth defects**
6
Includes aggregated data reported to the US Zika Pregnancy Registry as of July 14, 2016
Pregnancy Outcomes in the United States Territories
Liveborn infants with birth defects*
0
Includes aggregated data from the US territories reported to the US Zika Pregnancy Registry and data from Puerto Rico reported to the Zika Active Pregnancy Surveillance System as of July 14, 2016
Pregnancy losses with birth defects**
1
Includes aggregated data from the US territories reported to the US Zika Pregnancy Registry and data from Puerto Rico reported to the Zika Active Pregnancy Surveillance System as of July 14, 2016
What these numbers show
- These numbers reflect poor outcomes among pregnancies with laboratory evidence of possible Zika virus infection reported to the US Zika Pregnancy Registry.
- The number of live-born infants and pregnancy losses with birth defects are combined for the 50 US states, the District of Columbia, and the US territories. To protect the privacy of the women and children affected by Zika, CDC is not reporting individual state, tribal, territorial or jurisdictional level data.
- The poor birth outcomes reported include those that have been detected in infants infected with Zika before or during birth, including microcephaly, calcium deposits in the brain indicating possible brain damage, excess fluid in the brain cavities and surrounding the brain, absent or poorly formed brain structures, abnormal eye development, or other problems resulting from damage to brain that affects nerves, muscles and bones, such as clubfoot or inflexible joints.
What these new numbers do not show
- These numbers are not real time estimates. They will reflect the outcomes of pregnancies reported with any laboratory evidence of possible Zika virus infection as of 12 noon every Thursday the week prior; numbers will be delayed one week.
- These numbers do not reflect outcomes among ongoing pregnancies.
- Although these outcomes occurred in pregnancies with laboratory evidence of Zika virus infection, we do not know whether they were caused by Zika virus infection or other factors.
Where do these numbers come from?
- These data reflect pregnancies reported to the US Zika Pregnancy Registry. CDC, in collaboration with state, local, tribal and territorial health departments, established this registry for comprehensive monitoring of pregnancy and infant outcomes following Zika virus infection.
- The data collected through this system will be used to update recommendations for clinical care, to plan for services and support for pregnant women and families affected by Zika virus, and to improve prevention of Zika virus infection during pregnancy.
These registries are covered by an assurance of confidentiality. This protection requires us to safeguard the information collected for the pregnant women and infants in the registries.
* Includes microcephaly, calcium deposits in the brain indicating possible brain damage, excess fluid in the brain cavities and surrounding the brain, absent or poorly formed brain structures, abnormal eye development, or other problems resulting from damage to the brain that affects nerves, muscles and bones, such as clubfoot or inflexible joints.
**Includes miscarriage, stillbirths, and terminations with evidence of the birth defects mentioned above
The Florida Department of Health announced that it is conducting an epidemiological investigation into a possible non-travel related case of Zika virus in Broward County.
Saturday, July 23rd, 2016Health officials on Friday reported the first baby born in New York City with the Zika-related birth defect known as microcephaly
Saturday, July 23rd, 2016“….For a pregnant woman infected with Zika, there is between a 1 percent and 29 percent chance her baby will be born with microcephaly. The wide range reflects the lack of scientific knowledge on the subject. There is no cure for Zika and health officials estimate that it will cost upward of $10 million for every child born with birth defects…..”
The Florida Department of Health is conducting an investigation into a possible non-travel related case of Zika virus in Miami-Dade County.
Thursday, July 21st, 2016July 19, 2016
Department of Health
Investigating Possible Non-Travel Related Case of Zika

Contact:
Communications Office
NewsMedia@flhealth.gov
(850) 245-4111
Tallahassee, Fla. — Today the Florida Department of Health announced that it is conducting an investigation into a possible non-travel related case of Zika virus in Miami-Dade County.
The department is actively conducting an epidemiological investigation, is collaborating with the Centers for Disease Control and will share additional details as they become available. Zika prevention kits and repellant will be available for pickup at DOH-Miami-Dade and distributed in the area under investigation. Zika kits are intended for pregnant women. Mosquito control has already conducted reduction and prevention activities in the area of investigation.
Residents and visitors are reminded that the best way to protect themselves is to prevent mosquito bites through practicing good drain and cover methods:
DRAIN standing water to stop mosquitoes from multiplying
- Drain water from garbage cans, house gutters, buckets, pool covers, coolers, toys, flower pots or any other containers where sprinkler or rain water has collected.
- Discard old tires, drums, bottles, cans, pots and pans, broken appliances and other items that aren’t being used.
- Empty and clean birdbaths and pet’s water bowls at least once or twice a week.
- Protect boats and vehicles from rain with tarps that don’t accumulate water.
- Maintain swimming pools in good condition and appropriately chlorinated. Empty plastic swimming pools when not in use.
COVER skin with clothing or repellent
- CLOTHING – Wear shoes, socks, long pants and long-sleeves. This type of protection may be necessary for people who must work in areas where mosquitoes are present.
- REPELLENT – Apply mosquito repellent to bare skin and clothing.
- Always use repellents according to the label. Repellents with DEET, picaridin, oil of lemon eucalyptus, and IR3535 are effective.
- EPA-approved repellent is safe for pregnant women to use.
- Use mosquito netting to protect children younger than 2 months old.
COVER doors and windows with screens to keep mosquitoes out of your house
- Repair broken screening on windows, doors, porches and patios.
The department continues to issue daily updates each week day at 2 p.m. Updates include a CDC-confirmed Zika case count by county and information to better keep Floridians prepared.
For more information on Zika virus, click here.
About the Florida Department of Health
The department, nationally accredited by the Public Health Accreditation Board, works to protect, promote and improve the health of all people in Florida through integrated state, county and community efforts.
Follow us on Twitter at @HealthyFla and on Facebook. For more information about the Florida Department of Health please visit www.FloridaHealth.gov.
A CDC Emergency Response Team (CERT) comes to Utah to investigate an unusual Zika case.
Tuesday, July 19th, 2016CDC is assisting in the investigation of a case of Zika in a Utah resident who is a family contact of the elderly Utah resident who died in late June. The deceased patient had traveled to an area with Zika and lab tests showed he had uniquely high amounts of virus—more than 100,000 times higher than seen in other samples of infected people—in his blood. Laboratories in Utah and at the Centers for Disease Control and Prevention (CDC) reported evidence of Zika infection in both Utah residents.
State and local public health disease control specialists, along with CDC, are investigating how the second resident became infected. The investigation includes additional interviews with and laboratory testing of family members and health care workers who may have had contact with the person who died and trapping mosquitoes and assessing the risk of local spread by mosquitoes.
A CDC Emergency Response Team (CERT) is in Utah at the request of the Utah Department of Health. The team includes experts in infection control, virology, mosquito control, disease investigation, and health communications.
“The new case in Utah is a surprise, showing that we still have more to learn about Zika,” said Erin Staples, MD, PhD, CDC’s Medical Epidemiologist on the ground in Utah. “Fortunately, the patient recovered quickly, and from what we have seen with more than 1,300 travel-associated cases of Zika in the continental United States and Hawaii, non-sexual spread from one person to another does not appear to be common.”
As of July 13, 2016, 1,306 cases of Zika have been reported in the continental United States and Hawaii; none of these have been the result of local spread by mosquitoes. These cases include 14 believed to be the result of sexual transmission and one that was the result of a laboratory exposure.
Since early 2016, CDC has worked with state, local, and territorial public health officials to protect pregnant women from Zika infection, through these activities:
- Alerts to pregnant women to avoid travel to an area with active Zika transmission, to women in these areas to take steps to prevent mosquito bites, and to partners of pregnant women to use a condom to prevent sexual transmission during pregnancy.
- Development and distribution of PCR and IgM testing kits to confirm Zika virus infection.
- Establishment of CDC Emergency Response Teams to rapidly deploy to assist with Zika-related preparedness and response activities in the United States.
- Deployment of experts to assist in enhancement of mosquito surveillance and testing.
- Collaboration with FDA, blood collection centers, and other entities in the public and private sectors on enhancement of surveillance of blood donations.
- Guidance to prevent sexual transmission, particularly to women who are pregnant.
- Guidance for clinicians on the care of pregnant women who may have been exposed to Zika.
Studies in collaboration with Brazil, Colombia, and other countries to better understand the link between Zika infection and birth defects, including microcephaly.
For more information about Zika: http://www.cdc.gov/zika/.
How did the caregiver from Utah contract Zika? Simple contact with a Zika family member?
Tuesday, July 19th, 2016https://www.youtube.com/watch?v=CwYJbyRO6Xc
Utah’s Unique Case of Zika: How did he get it?
Tuesday, July 19th, 2016Monday, July 18, 2016
Public Health Officials Investigating Unique Case of Zika
Salt Lake County Health Department


