Archive for February, 2017
Predictive and easy-to-use prognostic tools, which stratify the risk of EVD mortality at or after EVD triage.
Saturday, February 4th, 2017PLOS: Hartley M-A, Young A, Tran A-M, Okoni-Williams HH, Suma M, Mancuso B, et al. (2017) Predicting Ebola Severity: A Clinical Prioritization Score for Ebola Virus Disease. PLoS Negl Trop Dis 11(2): e0005265. doi:10.1371/journal.pntd.0005265
- 158 Ebola patients: Study population
- The authors were able to accurately predict death at triage 91% of the time and death after triage 97% of the time.
- Co-infection with malaria was associated with a 2.5-fold increase in the odds of death.
- Disorientation, hiccups, diarrhea, conjunctivitis, shortness of breath, and muscle aches were also strong predictors of death.
- Age was also a predictor of mortality.
- The patient group aged between 5 and 24 years had the lowest mortality rate of 42.5%
- The over-45’s and under-5’s were particularly vulnerable, being 11.6 and 5.4 fold more likely to die, respectively.
Background
Methods/Principal Findings
This retrospective cohort study analyses the clinical characteristics of 158 EVD(+) patients at the GOAL-Mathaska Ebola Treatment Centre, Sierra Leone. The prognostic potential of each characteristic was assessed and incorporated into a statistically weighted disease score. The mortality rate among EVD(+) patients was 60.8% and highest in those aged <5 or >25 years (p<0.05). Death was significantly associated with malaria co-infection (OR = 2.5, p = 0.01). However, this observation was abrogated after adjustment to Ebola viral load (p = 0.1), potentially indicating a pathologic synergy between the infections. Similarly, referral-time interacted with viral load, and adjustment revealed referral-time as a significant determinant of mortality, thus quantifying the benefits of early reporting as a 12% mortality risk reduction per day (p = 0.012). Disorientation was the strongest unadjusted predictor of death (OR = 13.1, p = 0.014) followed by hiccups, diarrhoea, conjunctivitis, dyspnoea and myalgia. Including these characteristics in multivariate prognostic scores, we obtained a 91% and 97% ability to discriminate death at or after triage respectively (area under ROC curve).
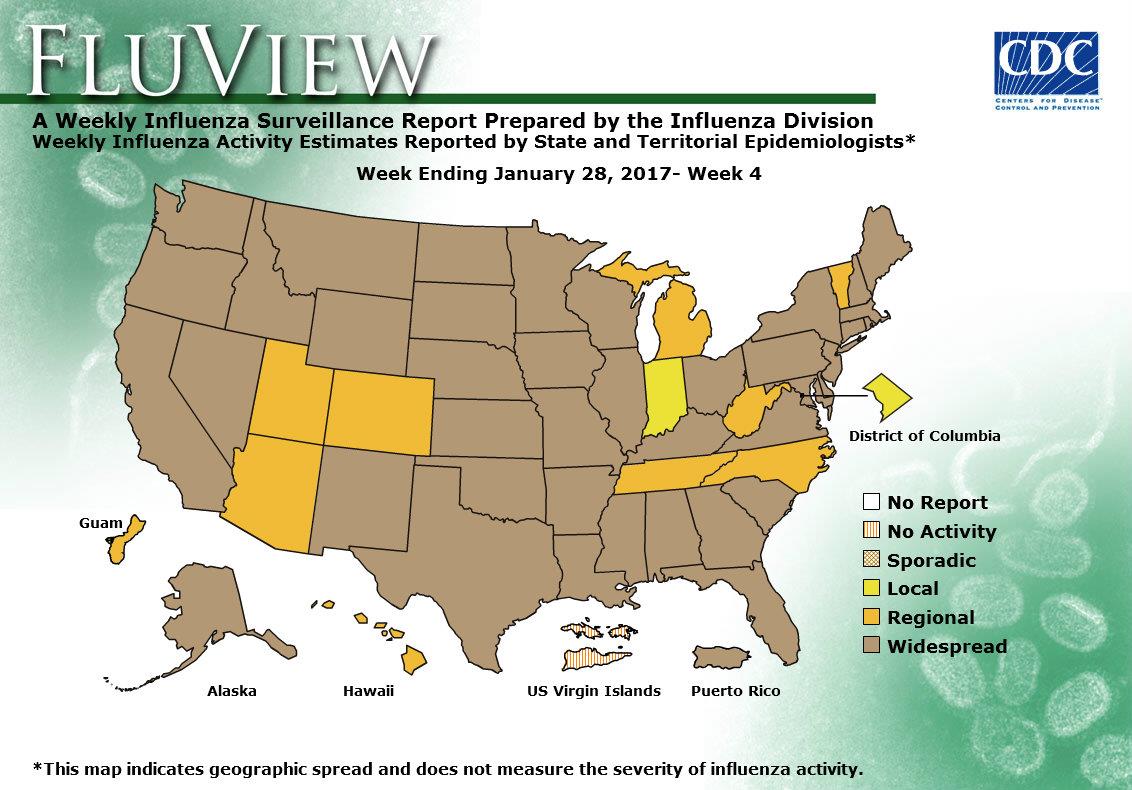
2016-2017 Influenza Season Week 4 ending January 28, 2017
Saturday, February 4th, 2017CDC Synopsis:
During week 4 (January 22-28, 2017), influenza activity increased in the United States.
- Viral Surveillance: The most frequently identified influenza virus subtype reported by public health laboratories during week 4 was influenza A (H3). The percentage of respiratory specimens testing positive for influenza in clinical laboratories increased.
- Pneumonia and Influenza Mortality: Due to data processing problems, the National Center for Health Statistics (NCHS) mortality surveillance data for the week ending January 14, 2015 (week 2) will not be published this week.
- Influenza-associated Pediatric Deaths: Seven influenza-associated pediatric deaths were reported.
- Influenza-associated Hospitalizations: A cumulative rate for the season of 20.3 laboratory-confirmed influenza-associated hospitalizations per 100,000 population was reported.
- Outpatient Illness Surveillance:The proportion of outpatient visits for influenza-like illness (ILI) was 3.9%, which is above the national baseline of 2.2%. All 10 regions reported ILI at or above their region-specific baseline levels. New York City and 15 states experienced high ILI activity; Puerto Rico and 11 states experienced moderate ILI activity; 14 states experienced low ILI activity; 10 states experienced minimal ILI activity, and the District of Columbia had insufficient data.
- Geographic Spread of Influenza: The geographic spread of influenza in Puerto Rico and 40 states was reported as widespread; Guam and nine states reported regional activity; the District of Columbia and one state reported local activity; and the U.S. Virgin Islands reported no activity.
Seven influenza-associated pediatric deaths were reported to CDC during week 4. Three deaths were associated with an influenza A (H3) virus and occurred during weeks 1, 2, and 4 (the weeks ending January 7, 14, and 28, 2017, respectively). Three deaths were associated with an influenza A virus for which no subtyping was performed and occurred during weeks 1, 3, and 4 (the weeks ending January 7, 21, and 28, 2017, respectively). One death was associated with an influenza B virus and occurred during week 3 (the week ending January 21, 2017).
A total of 15 influenza-associated pediatric deaths have been reported for the 2016-2017 season.
Brazil: The number of confirmed cases of Yellow Fever in Minas Gerais rose to 109
Friday, February 3rd, 2017
New quarantine rules: CDC trying to out-Trump Trump. And that’s making people jumpy…..
Thursday, February 2nd, 2017“….Under the old rules, the CDC’s authority was primarily limited to detaining people entering the country or crossing state lines. The agency was also limited to quarantining people who had one of about a dozen diseases, including cholera, diphtheria, tuberculosis, plague, smallpox and yellow fever.
Yet even then, the CDC rarely exercised these powers and generally deferred to state and local health officials.
With the new rules, the CDC would be able to detain people anywhere in the country without getting approval from state and local officials.
The agency could also apprehend people to assess their health if they are exhibiting medical problems such as a high fever, headache, cramps and other symptoms that could be indicative of a dangerous infectious disease…..”
Afghanistan: Over 5.6 million children to be vaccinated against polio during large-scale vaccination campaign
Thursday, February 2nd, 2017Kabul 30 January 2017 – The Ministry of Public Health, WHO and UNICEF launched today the first polio subnational immunization days campaign of 2017. Over 5.6 million children will be vaccinated against polio in all provinces in the southern and south-eastern regions, most districts in the eastern region, as well as selected high-risk districts across the country, including Kabul city.

“The campaign will build on strong progress seen in 2016. Last year Afghanistan had only 13 cases of polio nationwide, down from 20 in 2015. This was made possible through hard work by thousands of frontline health workers and a renewed emphasis on monitoring and oversight,” said Dr Maiwand Ahmadzai, Director of the National Emergency Operations Centre for Polio Eradication at the Ministry of Public Health, speaking at a joint press conference held in Kabul.
This week’s campaign is carried out by over 31 000 trained polio workers and it runs until 3 February when vaccinators revisit children who were missed when the vaccinators first visited. These vaccinators and other polio workers are trusted members of the community and they have been chosen because they care about children.
“We have seen significant progress in our polio eradication efforts over the past year. Most of Afghanistan is now polio-free, the circulation of the poliovirus is restricted to small areas in the eastern, southern and southeastern parts of the country and we have seen huge improvements in vaccination campaign quality,” said Dr Hemant Shukla, director of the polio programme at WHO. “Our focus is now on reaching every single child during every vaccination campaign to stop the transmission of polio.”
“With our collective efforts, we will be able to eradicate polio from the world. Vaccines are the right of every child and no child should be missed during polio campaigns,” said Ms Melissa Corkum, UNICEF Polio director in Afghanistan. “Thousands of frontline workers visit every house in the country during campaigns. That’s not an easy task. Due to the hard work of these dedicated frontline workers, we are closer to polio eradication than ever.”
In 2016, new initiatives have been implemented to strengthen the polio eradication programme in Afghanistan. All polio eradication activities have been brought under one leadership as Emergency Operations Centres have been established at the national and subnational level. The surveillance system has been strengthened and the circulation of wild poliovirus is unlikely to be missed in Afghanistan. The quality of campaigns, routine immunization and rapid response to polio cases have improved tremendously over the past year.
In 2016, 13 polio cases were registered: 7 cases in Paktika, 4 cases in Kunar, one case in Kandahar and one in Helmand province. Afghanistan remains one of 3 polio-endemic countries together with Pakistan and Nigeria.
5 cases of culture-confirmed human plague treated successfully with oral ciprofloxacin
Thursday, February 2nd, 2017Abstract: “The US Food and Drug Administration recently approved ciprofloxacin for treatment of plague (Yersina pestis infection) based on animal studies. Published evidence of efficacy in humans is sparse. We report 5 cases of culture-confirmed human plague treated successfully with oral ciprofloxacin, including 1 case of pneumonic plague.”
Apangu T, Griffith K, Abaru J, Candini G, Apio H, Okoth F, et al. Successful treatment of human plague with oral ciprofloxacin. Emerg Infect Dis. 2017 Mar [date cited]. http://dx.doi.org/10.3201/eid2303.161212
Demographic and clinical characteristics of 5 patients with culture-confirmed plague (Yersina pestis infection) who were treated successfully with oral ciprofloxacin, Uganda, 2011–2014
| Patient no. | Age, y/sex | Length of illness, d* | Symptoms | Laboratory evidence | Ciprofloxacin dose, mg† |
|---|---|---|---|---|---|
| 1 | 10/F | 7 | Fever, left axillary bubo | Bubo, blood cultures positive | 250 |
| 2 | 52/F | 4 | Fever, right axillary bubo | Bubo, blood cultures positive | 650 |
| 3 | 27/F | 1 | Fever, left inguinal bubo | Bubo, blood cultures positive | 750 |
| 4 | 36/M | 1 | Fever, left axillary bubo | Blood culture positive | 625 |
| 5 | 13/M | 6 | Fever, chest pain, cough, blood-tinged sputum | Sputum culture positive, blood culture negative | 375 |
*At time treatment was sought.
†Orally, twice daily; ≈15 mg/kg bodyweight with a maximum of 750 mg.
Pneumonic plague persists as a threat in Madagascar, where poor healthcare systems and traditional burial practices promote these outbreaks.
Thursday, February 2nd, 2017Abstract: “During a pneumonic plague outbreak in Moramanga, Madagascar, we identified 4 confirmed, 1 presumptive, and 9 suspected plague case-patients. Human-to-human transmission among close contacts was high (reproductive number 1.44) and the case fatality rate was 71%. Phylogenetic analysis showed that the Yersinia pestis isolates belonged to group q3, different from the previous outbreak.”
Ramasindrazana B, Andrianaivoarimanana V, Rakotondramanga JM, Birdsell DN, Ratsitorahina M, Rajerison M. Pneumonic plague transmission, Moramanga, Madagascar, 2015. Emerg Infect Dis. 2017 Mar [date cited]. http://dx.doi.org/10.3201/eid2303.161406
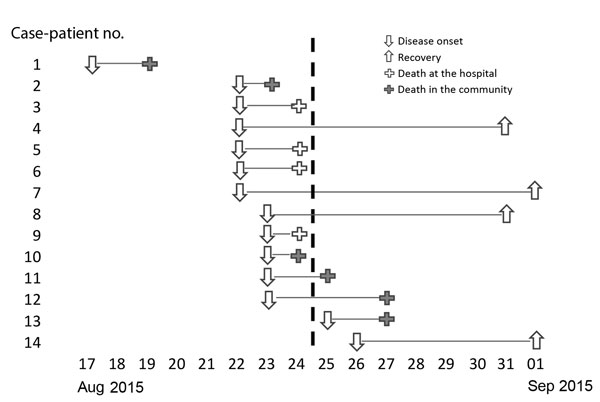
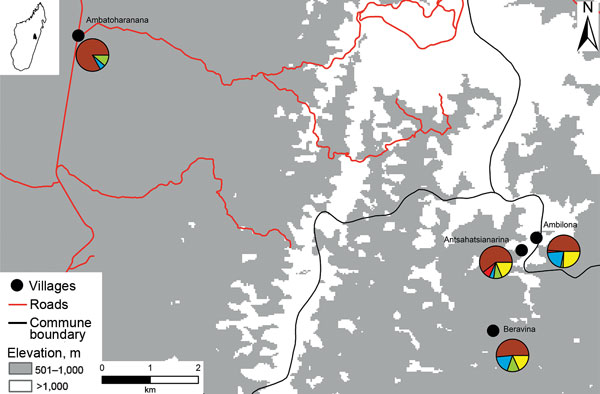
Map of pneumonic plague outbreak (n = 14) in the commune of Ampasipotsy Gara in Moramanga, Madagascar, 2015. The index case-patient (case-patient 1) was infected with Yersinia pestis at Antsahatsianarina and spread the bacterium to Beravina (burial site of case-patient 1), Ambilona (case-patient 10’s home), and Ambatoharanana (burial site of case-patient 2 and home of case-patient 14). Each pie chart indicates the proportions of plague cases (red), seropositive contacts (blue), seronegative contacts (green), unsampled contacts (yellow), and noncontacts (brown) among the total inhabitants of each site.
Drones & ISIS: Could it happen here as a weapon of terror?
Wednesday, February 1st, 2017“….In the past two months, the Islamic State has used more than 80 remotely piloted drones against Iraqi forces and their allies. About one-third of the aircraft, some as small as model airplanes, dropped bombs or were rigged with explosives to detonate on the ground……