Archive for May, 2017
Ongoing Transmission of Candida auris in Health Care Facilities — United States, June 2016–May 2017.
Friday, May 19th, 2017
Tsay S, Welsh RM, Adams EH, et al. Notes from the Field: Ongoing Transmission of Candida auris in Health Care Facilities — United States, June 2016–May 2017. MMWR Morb Mortal Wkly Rep 2017;66:514–515. DOI: http://dx.doi.org/10.15585/mmwr.mm6619a7.
2016-2017 Influenza Season Week 19 ending May 13, 2017
Friday, May 19th, 2017Synopsis:
During week 19 (May 7-13, 2017), influenza activity decreased in the United States.
- Viral Surveillance: The most frequently identified influenza virus type reported by public health laboratories during week 19 was influenza B. The percentage of respiratory specimens testing positive for influenza in clinical laboratories decreased.
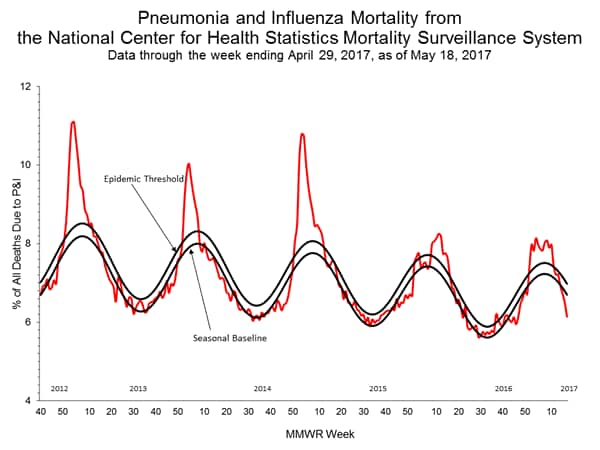
- Pneumonia and Influenza Mortality: The proportion of deaths attributed to pneumonia and influenza (P&I) was below the system-specific epidemic threshold in the National Center for Health Statistics (NCHS) Mortality Surveillance System.
- Influenza-associated Pediatric Deaths: One influenza-associated pediatric death was reported.
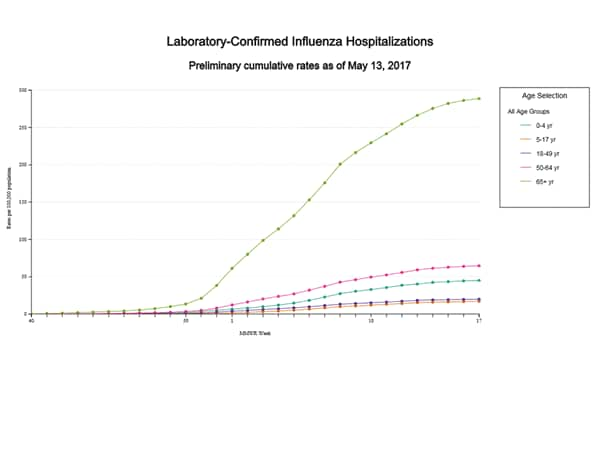
- Influenza-associated Hospitalizations: A cumulative rate for the season of 64.7 laboratory-confirmed influenza-associated hospitalizations per 100,000 population was reported.
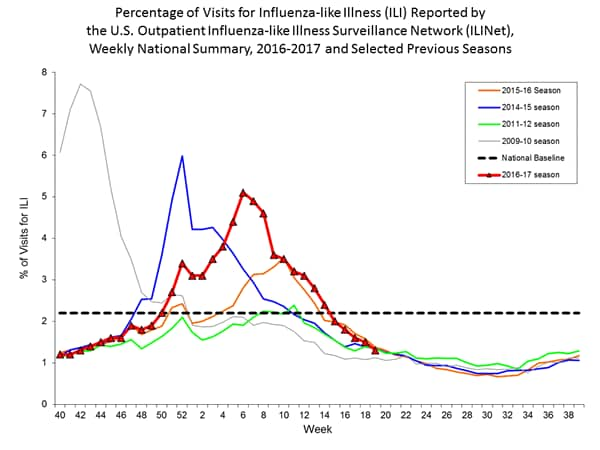
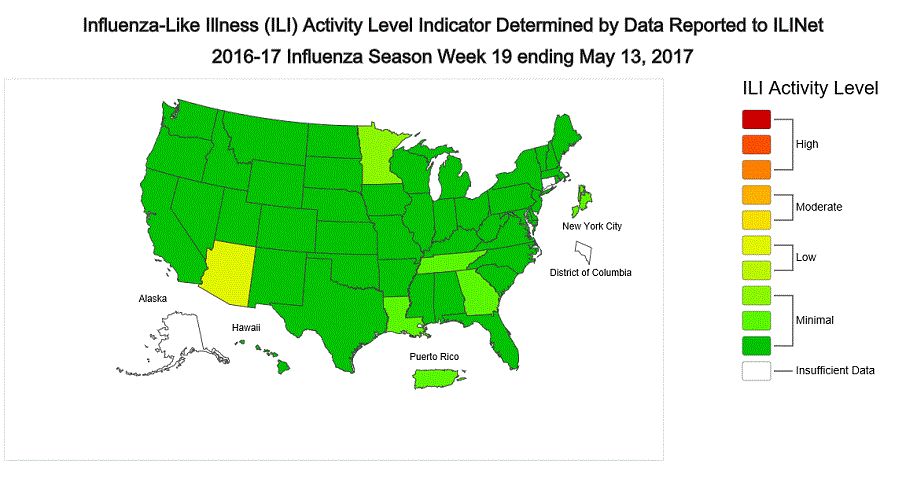
- Outpatient Illness Surveillance: The proportion of outpatient visits for influenza-like illness (ILI) was 1.3%, which is below the national baseline of 2.2%. All ten regions reported ILI below their region-specific baseline levels. One state experienced low ILI activity; New York City, Puerto Rico, and 47 states experienced minimal ILI activity; and the District of Columbia and two states had insufficient data.
- Geographic Spread of Influenza: The geographic spread of influenza in Guam and five states was reported as regional activity; Puerto Rico and eight states reported local activity; the District of Columbia and 36 states reported sporadic activity; and the U.S. Virgin Islands and one state reported no activity.
NYC’s Unified Victim Identification System (UVIS)
Friday, May 19th, 2017Unified Victim Identification System (UVIS) document: UVIS Information Guide-NYC
“…..In concert with the City’s 311-call center, UVIS enables a centralized communications and data collection processes to support the family assistance center (FAC). This coordinated system is essential to developing an accurate manifest of potential victims – a critical step in victim identification. Most importantly, the coordinated UVIS-311 call center system keeps the lines of communication open to the families, friends and associates of possible victims. Such a resource is invaluable in the chaos that follows any tragic event…..
UVIS is designed to handle multiple types of scenarios, and can manage up to 156 simultaneous events if needed. For example a terrorist operation may target different discrete areas of a large city (multiple incidents), as was the case on July 7th 2005 when a series of coordinated bomb blasts hit London’s public transport system during the morning rush hour resulting in more that 121,000 call center reports.
Most importantly, UVIS enables the OCME to meet its primary objectives following a catastrophic incident. They include:
• Investigate, Recover & Process Decedents in a Dignified and Respectful Manner
• Accurately Determine Cause & Manner of Death
• Perform Accurate & Efficient Identification of Victims
• Provide Families with Factual & Timely Information in a Compassionate Manner
• Conduct Rapid Return of Victims to their Legal Next of Kin ……..”
Times Square Slayer: “You were supposed to shoot me! I wanted to kill them.”
Friday, May 19th, 2017“…The killer, who has been arrested twice for drunken driving, was heading south on Seventh Avenue at 11:55 a.m. when he pulled a sudden U-turn at West 42nd Street, then barreled north — the wrong way — sending victims flying and witnesses running for their lives.
Rojas, of The Bronx, finally crashed his Honda Accord into a stanchion at Broadway and 45th Street — then got out of the car and ran toward a group of people with his arms outstretched before being tackled by law enforcement, including a transit cop and an FBI agent….”
An 18-year-old woman was killed and at least 22 people injured Thursday when a speeding car plowed into pedestrians in Manhattan’s bustling Times Square
Thursday, May 18th, 2017https://www.youtube.com/watch?v=sE7PFubIraw
Movements during routine nursing procedures can increase the risk of face seal leakage of N95 respirators, according to a study that involved nursing students who wore backpack aerosol spectrometers that measured particles that entered the mask.
Thursday, May 18th, 2017Highlights
- •N95 respirators, although adequately fitted, may not provide consistent protection for users.
- •Movements during nursing procedures can significantly increase the risk of face seal leakage.
- •Improvements in respirator design to minimize face seal leakage are essential.
- •Portable aerosol spectrometers offer a reliable method for real-time measurement of N95 mask fit.
Background
The adequate fit of an N95 respirator is important for health care workers to reduce the transmission of airborne infectious diseases in the clinical setting. This study aimed to evaluate whether adequately sealed N95 respirators may provide consistent protection for the wearer while performing nursing procedures.
Methods
Participants were a group of nursing students (N = 120). The best fitting respirator for these participants was identified from the 3 common models, 1860, 1860S, and 1870+ (3M), using the quantitative fit test (QNFT) method. Participants performed nursing procedures for 10-minute periods while wearing a backpack containing the portable aerosol spectrometers throughout the assessment to detect air particles inside the respirator.
Results
The average fit factor of the best fitting respirator worn by the participants dropped significantly after nursing procedures (184.85 vs 134.71) as detected by the QNFT. In addition, significant differences in particle concentration of different sizes (>0.3, >0.4, >1.0, and >4.0 µm) inside the respirator were detected by the portable aerosol spectrometers before, during, and after nursing procedures.
Conclusions
Body movements during nursing procedures may increase the risk of face seal leakage. Further research, including the development of prototype devices for better respirator fit, is necessary to improve respiratory protection of users.
WHO said 2 new suspected Ebola cases are being investigated in the Democratic Republic of Congo (DRC), and a US expert says events are unfolding in ways reminiscent of Guinea in 2014 at the onset of a massive West Africa outbreak.
Thursday, May 18th, 20171. Situation update
WHO continues to monitor the outbreak of Ebola virus disease (EVD) in Likati Health Zone, Bas Uele Province located in the north-east of the Democratic Republic of the Congo. Between 15 May and 16 May 2017, two new suspected EVD cases were reported in Azande (one case) and Nambwa (1 case) health areas in Lakati Health Zone. As of 16 May 2017, 21 suspected EVD cases including three deaths (case fatality rate of 14.3%) have been reported. Most of the cases presented with fever, vomiting, bloody diarrhoea and other bleeding symptoms and signs. The cases have been reported from four health areas, namely Nambwa (13 cases and two deaths), Mouma (three cases and one death), Ngayi (four cases and no deaths) and Azande (one case and no deaths).
Two of five blood samples collected from the initial cases and analysed at the Institut National de Recherche Biomédicale (INRB) laboratory in Kinshasa tested positive for Zaire ebolavirus. Approximately 400 close contacts have been registered in Likati Health Zone and are being monitored.
This Ebola outbreak in the Democratic Republic of the Congo was notified to WHO by the Ministry of Health on 11 May 2017. The cluster of cases and deaths of previously unidentified illness have been reported since late April 2017. Likati Health Zone shares borders with two provinces in the Democratic Republic of the Congo and with the Central African Republic (Fig. 1). The affected areas are remote and hard to reach, with limited communication and transport networks.
EBOLA VIRUS DISEASE Democratic Republic of Congo
Date of issue: 16 May 2017
The current outbreak is the eighth Ebola outbreak in the Democratic Republic of the Congo since the disease was first discovered in 1976 in Yambuku.
Health Emergency Information and Risk Assessment Health Emergency Information and Risk Assessment 2-19 suspected cases -3 deaths
As this is a rapidly changing situation, the number of reported cases and deaths, contacts under medical observation and the number of laboratory results are subject to change due to enhanced surveillance and contact tracing activities, ongoing laboratory investigations and consolidation of case, contact and laboratory data.
Health Emergency Information and Risk Assessment Health Emergency Information and Risk Assessment 3
Current risk assessment
• The risk is high at the national level due to the known impact of Ebola outbreaks, remoteness of the affected area, limited access to health care and suboptimal surveillance. • Risk at the regional level is moderate due to the proximity of international borders and the recent influx of refugees from Central African Republic. • The risk is low at global level due to the remoteness and inaccessibility of the area to major international ports.
The risk assessment will be revaluated by the three levels of WHO according to the evolution of the situation and the available information. WHO advises against the application of any travel or trade restrictions on the Democratic Republic of the Congo based on the currently available information. WHO continues to monitor reports of measures being implemented at points of entry.
WHO’s strategic approach to the prevention, detection and control of EVD
WHO recommends the implementation of strategies that have proven to be effective in preventing and control of Ebola outbreaks. These strategies include (i) coordination of the response, (ii) enhanced surveillance, (iii) laboratory confirmation, (iv) contact identification and follow-up, (v) case management, (vi) infection prevention and control, (vii) safe burials, (viii) social mobilization and community engagement, (ix) logistics, (x) risk communication, (xi) vaccination, (xii) partner engagement, (xiii) research and (xiv) resource mobilization.
2. Actions to date
Since the declaration of the outbreak, the WHO regional Office for Africa, as well as the other levels of WHO, are providing a high level of support to the country in order to ensure an effective response to this event.
Coordination of the response
• On 15 May 2017, the Minister of Public Health chaired the Health Emergency Management Committee meeting in Kinshasa which was attended by government officials and partners. The attendees reviewed the current situation, discussed strategies and planned the implementation of control interventions. • The national, provincial and zonal response teams, in collaboration with partners, are conducting daily coordination meetings in order to design strategies, plan, implement and monitor progress of the response. • WHO is conducting daily conference calls involving all the three levels of WHO to strategize and provide guidance.
Surveillance
• The national rapid response team arrived in Likati Health Zone on 15 May 2017. The team will conduct detailed epidemiological investigations and support the local response. • Active surveillance is being established and strengthened in the affected region and daily reporting has been implemented. Surveillance is also being enhanced nationwide.
Laboratory confirmation
• By 15 May 2017, five new blood samples have been collected from the affected people and are being transported to the Institut National de Recherche Biomédicale (INRB) laboratory in Kinshasa for testing. • INRB is deploying 2 mobile laboratories to Buta and Likati. There is additional mobile laboratory support available through GOARN/EDPLN for if required. • The available samples will be transported to the WHO Collaborating Centre for further analysis. • Samples transportation mechanism from the field is being improved to enable timely confirmation of suspected cases.
Health Emergency Information and Risk Assessment Health Emergency Information and Risk Assessment 4
Health Emergency Information and Risk Assessment Health Emergency Information and Risk Assessment 5
Infection prevention and control / safe burials
• The disinfection of materials and homes of the cases is ongoing in Likati and Nambwa health zones. • The logistics and capacity to conduct safe burials are being put in place.
Contact identification and follow-up
• At least 400 contacts have been identified and are being followed up on a daily basis. Efforts are ongoing to establish and strengthen contact tracing mechanisms. • Tools for contact identification and follow up are being distributed to health workers.
Case management
• Preparations by the non-governmental organizations Médecins Sans Frontières (MSF) and the Alliance for International Medical Action (ALIMA) are ongoing to support the establishment of proper isolation and treatment facilities in the affected areas.
Social mobilization and community engagement
• National social mobilization and community engagement experts are on the ground to sensitize and engage the communities.
Logistic
• The logistics team in Kinshasa is working closely with logistics partners and stakeholders across the Democratic Republic of the Congo to ensure effective collaboration and coordination. The logistic issues to be addressed include supply, warehousing, transport, setting up of living quarters and operations base(s) in remote zones, setting up medical and isolation facilities, and referral of patients. The international logistics partners include UNICEF, World Food Programme (WFP), MSF, ALIMA, the United States Agency for International Development (USAID) and the United Kingdom Department for International Development (DFID). • WFP/Logistics Cluster and UNICEF have been approach to support warehousing capacity in Buta and eventually Likati. • WHO donated 3,000 sets of personal protective equipment (PPE), enough to support a facility of 30 beds for 30 days. The other supplies donated include 100 body bags, sprayers, chlorine powder for disinfection and infrared thermometers. The supplies have been transported to Likati. • Communication equipment, including satellite phones and data satellite communication devices has been deployed. • Discussions to secure air transport are in advanced stages. The options will include using both helicopter and fixed-wing flights. The United Nations Humanitarian Air Service (UNHAS) will set up a base to operate from Buta. •
Resources Mobilization
• The Ministry of Health has finalized the national Ebola outbreak response plan and budget, amounting to US$ 8 million. The response plan and budget has been presented and discussed with partners. • The WHO Country Office in the Democratic Republic of the Congo finalized a response plan and budget amounting to US$ 1.4 million. •
Risk communication
• Risk communication messages are being aired through local radio channels. Awareness campaigns are also being organized in markets, churches and other public places. • An advocacy meeting was held with the political and administrative authorities
Health Emergency Information and Risk Assessment Health Emergency Information and Risk Assessment 6
Partnership
• WHO continues to mobilize partners to provide technical and logistical support to the country. • GOARN Operational Support Team is coordinating Partner inputs and regular information sharing through teleconferences and secure Knowledge Platform. • MSF and ALIMA are on the ground in Likati to provide technical support.
IHR Travel measures
• As of 16 May 2017, three countries have instituted entry screening at airports and ports of entry (Nigeria, Tanzania, and Zimbabwe), and two countries have issued travel advisories to avoid unnecessary travel to DRC (Rwanda) or to areas around the epicenter of the epidemic (United Kingdom). • The IHR Secretariat, together with ICAO is actively monitoring the travel measures implemented by States Parties in relation to this outbreak. • WHO does not currently recommend any restrictions of travel and trade in relation to this outbreak.
3. Summary of public health risks, needs and gaps
The critical needs currently are access to the affected areas and to enable the timely deployment of required human and logistical resources, including the mobile laboratory and communication tools.
Proposed ways forward include:
• Establishing appropriate Ebola isolation and treatment facilities; • Initiate implementation of response interventions in all the essential pillars; • Continuing with the deployment of national and international experts to the affected areas; • Mobilizing needed resources, including telecommunications and air transport logistics, to ease communication and access to the affected areas.