Archive for July, 2017
The Ukraine’s Ministry of Health has said “as of July 18, 2017, 81 cases of botulism were reported in Ukraine, 90 people fell ill, nine of them fatally”.
Sunday, July 23rd, 2017ISIS was close: Locked away in a storage room on a Mosul college campus were two caches of cobalt-60 (the core ingredient of a “dirty bomb” ).
Sunday, July 23rd, 2017https://www.youtube.com/watch?v=kw3jcAujeY8
‘…..“The worst case would have been the Islamic State widely dispersing the radioactive cobalt in a city, causing panic and an expensive, disruptive cleanup,” said Albright, a nuclear weapons expert and former U.N. weapons inspector. “There would likely not have been that many deaths, but the panic could have been profound, leading to the emptying of parts of the city as residents fled, fearful of the effects of radiation.”….’
Kenya: As of Jul 17, a total of 1,216 suspected cholera cases including 14 deaths (case-fatality rate of 1.2%) have been reported since the first of the year.
Sunday, July 23rd, 2017Cholera – Kenya
Since the beginning of 2017, Kenya is experiencing an upsurge of cholera cases. The first cholera outbreak reported in 2017 was in Tana River County. The outbreak started on 10 October 2016 and was controlled by April 2017.

A second wave of cholera outbreaks started in Garissa County on 2 April 2017 and was reported later in nine other counties including Nairobi, Murang’a, Vihiga, Mombasa, Turkana, Kericho, Nakuru, Kiambu, and Narok. The outbreak is being reported in the general population and in refugee camps. In Garissa County, the outbreak is affecting mainly Dadaab refugee camps and cases and deaths are being reported from Hagadera, Dagahaleh, and IFO2 camps. In Turkana county, the disease is also affecting Kakuma and Kalobeyei refugee camps.
In addition to the outbreak reported in the general population, there have been two point source cholera outbreaks in Nairobi County. One occurred among participants attending a conference in a Nairobi hotel on 22 June 2017. A total of 146 patients associated with this outbreak have been treated in different hospitals in Nairobi. A second outbreak occurred at the China Trade Fair held at the KICC Tsavo Ball between 10 and 12 July 2017. A total of 136 cases were reported and one death.
Currently, the outbreak is active in two counties, namely Garissa and Nairobi. As of 17 July 2017, a total of 1216 suspected cases including 14 deaths (case fatality rate: 1.2%) have been reported since 1 January 2017. In the week ending 16 July 2017, a total of 38 cases with no deaths were reported.
A total of 124 cases tested positive for Vibrio cholerae in the reference laboratory. In the week ending 25 June 2017, 18 samples out of 25 tested positive for Vibrio cholerae Ogawa by culture at the National Public Health Laboratory in Nairobi.
The main causative factors of the current outbreak include the high population density that is conducive to the propagation and spread of the disease, mass gatherings (a wedding party held in Karen and in a hotel during an international conference), low access to safe water and proper sanitation and the massive population movements in country and with neighbouring countries.
Since December 2014, the Republic of Kenya has been experiencing continuous large outbreaks of cholera, with a cumulative total of 17 597 cases reported (10 568 cases reported in 2015 and 6448 in 2016).
Public health response
The country has activated the national task force to coordinate the response to the outbreak. Since January 2017, WHO and partners are providing technical support to the country for the control of the outbreak. The country will develop a response plan with focus on the preparedness interventions to avert further spread of the outbreak. The WHO country office will repurpose their staff members and experts deployed in Nairobi for the management of the post El Niño effects in the Horn of Africa to support the quick control of this outbreak. WHO will also support the five most at risk counties with disease surveillance and response coordination. Partners on the ground are committed to provide support to the ongoing response efforts including support to primary health care and social mobilization by United Nations Children’s Fund (UNICEF).
WHO risk assessment
Cholera is an acute enteric infection caused by the ingestion of bacterium Vibrio cholerae present in faecally contaminated water or food. It is primarily linked to insufficient access to safe water and adequate sanitation. Cholera is always considered a potentially serious infectious disease and can cause high morbidity and mortality. It has the potential to spread rapidly, depending on the exposure frequency, population exposed and the context.
Cholera outbreaks have been reported in the Republic of Kenya every year with large cyclical epidemics every five to seven years.
The risk of the current outbreak is assessed as high at national and regional levels and moderate at global level. The outbreak occurred in the context of a sub-regional drought, conflicts and insecurity in the Horn of Africa. In addition, the outbreak is affecting the densely populated capital city Nairobi, and two large refugee camps (Kakuma and Dadaab) with massive population movements within country and between neighbouring countries. Previous large outbreaks in the Republic of Kenya have originated from similar settings, and the risk for propagation of cholera within the affected area as well as to other parts of the country is high. The country has identified a limited capacity for response and low access to safe water. There is an opportunity to implement early preparedness and response measures to contain the outbreak and prevent spread.
The current outbreaks linked to mass gathering activities poses additional risk of food safety as well as the need to conduct sanitary inspection in restaurants and hotels.
WHO recommendations
WHO recommends improving the readiness of counties and health facilities to early detect and respond to the cholera outbreak as well as the reinforcement of coordination and multisectoral approaches. In addition, hygiene practices in households, restaurant, hotels, refugee camps and health facilities should be improved and food safety interventions should be strengthened.
WHO does not recommend any restriction on travel and trade to the Republic of Kenya based on the information available on the current outbreak.
Five additional laboratory-confirmed cases of human infection with avian influenza A(H7N9) virus in China.
Sunday, July 23rd, 2017Human infection with avian influenza A(H7N9) virus – China
On 19 June 2017, the National Health and Family Planning Commission of China (NHFPC) notified WHO of five additional laboratory-confirmed cases of human infection with avian influenza A(H7N9) virus in China. On 24 June 2017, the NHFPC notified WHO of 10 additional laboratory-confirmed cases of human infection with avian influenza A(H7N9) virus in China. On 30 June 2017, the NHFPC notified WHO of six additional laboratory-confirmed cases of human infection with avian influenza A(H7N9) virus in China.
Details of the case patients
On 19 June 2017, the NHFPC reported five laboratory-confirmed human cases of infection with avian influenza A(H7N9) virus in China. Onset dates ranged from 25 April to 6 June 2017. Of these five cases, one was female. The median age was 55 years (range 41 to 68 years). The case patients were reported from Beijing (1), Guangxi (1), Guizhou (1), Hunan (1), and Zhejiang (1). At the time of notification, there was one death. Four cases were diagnosed as having severe pneumonia. Three cases were reported to have had exposure to poultry or live poultry market, and two had no known poultry exposure. No case clustering was reported.
On 24 June 2017, the NHFPC reported 10 laboratory-confirmed human cases of infection with avian influenza A(H7N9) virus in China. Onset dates ranged from 5 to 19 June 2017. All cases were male. The median age was 53.5 years (range 31 to 79 years). The cases were reported from Anhui (1), Beijing (2), Guizhou (1), Hebei (1), Inner Mongolia (1), Jiangsu (1), Sichuan (2), and Tianjin (1). This is the first case reported in Inner Mongolia since the virus emerged in 2013 although two cases were recently reported from Shaanxi province but who had likely exposure in Inner Mongolia. At the time of notification, there were two deaths. Eight cases were diagnosed as having either pneumonia (4) or severe pneumonia (4). Nine cases were reported to have had exposure to poultry or live poultry market, and one had no known poultry exposure.
One cluster with two cases was reported and both cases are from Panzhihua City, Sichuan Province, and had exposure to the same live poultry market. The cluster includes:
- A 79-year-old male, who had symptom onset on 12 June 2017 and was admitted to hospital with severe pneumonia on 15 June 2017, then died on the 21 June 2017. He was living on an upper floor of the live poultry market and passed regularly through the market.
- A 48-year-old male, who had symptom onset on 7 June 2017 and was admitted to hospital with severe pneumonia on 11 June 2017. He is a seller of poultry at the same live poultry market.
On 30 June 2017, the NHFPC reported six laboratory-confirmed human cases of infection with avian influenza A(H7N9) virus in China. Onset dates ranged from 11 to 23 June 2017. Three cases were male. The median age was 37.5 years (range 4 to 72 years). The cases were reported from Guizhou (1), Shanxi (1), and Yunnan (4) provinces. At the time of notification no associated deaths were reported. Four cases were diagnosed as having either pneumonia (1) or severe pneumonia (3). Two mild cases, identified through ILI surveillance, were reported: one in a child with exposure to market poultry and one in an adult. Five cases were reported to have had exposure to poultry or live poultry market, and one had no known poultry exposure. These are the first cases reported with exposure to the virus in Yunnan province. Previous cases reported from Yunnan province had likely exposure in a neighbouring province.
One cluster with two cases was reported, which include:
- A 33-year-old female from Wenshan, Yunnan Province had symptom onset on 17 June 2017 and was admitted to hospital with severe pneumonia on the same day. She had no apparent exposure to live poultry.
- Her sister-in-law, a 42-year-old female also from Wenshan, Yunnan Province, visited her in the hospital, developed mild symptoms on 21 June and was hospitalized on 24 June 2017. Investigation of the case revealed that she ran a shop near a live poultry market and bought live poultry from the market on a daily basis before her symptom onset. The investigation concluded that the likely source of her infection was exposure to the virus from visiting live poultry markets.
To date, a total of 1554 laboratory-confirmed human infections with avian influenza A(H7N9) virus have been reported through IHR notification since early 2013.
Public health response
The Chinese government at national and local level is taking preventive measures which include:
- Continuing to guide the provinces to strengthen assessment, and prevention and control measures.
- Continuing to strengthen control measures focusing on hygienic management of live poultry markets and cross-regional transportation.
- Conducting detailed source investigations to inform effective prevention and control measures.
- Continuing to detect and treat human infections with avian influenza A(H7N9) early to reduce mortality.
- Continuing to carry out risk communication and issue information notices to provide the public with guidance on self-protection.
- Strengthening virology surveillance to better understand levels of virus contamination in the environment as well as mutations, in order to provide further guidance for prevention and control.
WHO risk assessment
The number of human infections with avian influenza A(H7N9) virus and the geographical distribution in the fifth epidemic wave (i.e. onset since 1 October 2016) is greater than earlier waves. This suggests that the virus is spreading, and emphasizes that further intensive surveillance and control measures in both human and animal health sector are crucial.
According to the epidemiological curve, the number of reported cases on a weekly basis seems to have peaked in early February and is slowly decreasing. The peak in cases this year corresponds to the timing of the peak in cases in previous years.
Most human cases are exposed to avian influenza A(H7N9) virus through contact with infected poultry or contaminated environments, including live poultry markets. Since the virus continues to be detected in animals and environments, and live poultry vending continues, further human cases can be expected. Additional sporadic human cases of avian influenza A(H7N9) in other provinces in China that have not yet reported human cases are also expected. Similarly, sporadic human cases of avian influenza A(H7N9) detected in countries bordering China would not be unexpected. Although small clusters of cases of human infection with avian influenza A(H7N9) virus have been reported including those involving patients in the same ward, current epidemiological and virological evidence suggests that this virus has not acquired the ability of sustained transmission among humans. Therefore the likelihood of further community level spread is considered low.
Close analysis of the epidemiological situation and further characterization of the most recent viruses are critical to assess associated risk and to adjust risk management measures in a timely manner.
WHO advice
WHO advises that travellers to countries with known outbreaks of avian influenza should avoid, if possible, poultry farms, contact with animals in live poultry markets, entering areas where poultry may be slaughtered, or contact with any surfaces that appear to be contaminated with faeces from poultry or other animals. Travellers should also wash their hands often with soap and water, and follow good food safety and good food hygiene practices.
WHO does not advise special screening at points of entry with regard to this event, nor does it currently recommend any travel or trade restrictions. As always, a diagnosis of infection with an avian influenza virus should be considered in individuals who develop severe acute respiratory symptoms while travelling in or soon after returning from an area where avian influenza is a concern.
WHO encourages countries to continue strengthening influenza surveillance, including surveillance for severe acute respiratory infections (SARI) and influenza-like illness (ILI) and to carefully review any unusual patterns, ensure reporting of human infections under the IHR 2005, and continue national health preparedness actions.
Salmonella Kiambu Infections Linked to Yellow Maradol Papayas: 47 ill in 12 States & 1 Death
Saturday, July 22nd, 2017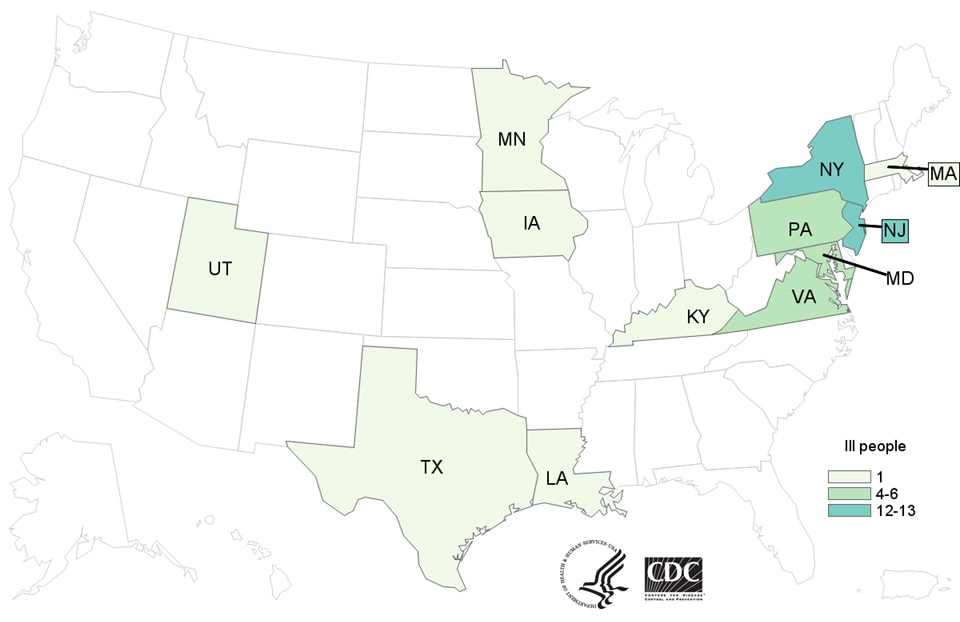
What are the signs and symptoms of Salmonella infection?
Most people infected with Salmonella develop the following signs and symptoms 12-72 hours after being exposed to the bacteria:
- Diarrhea
- Fever
- Abdominal cramps
How long does the illness last?
- The illness usually lasts 4 to 7 days, and most people recover without treatment.
- In some people, the diarrhea may be so severe that the patient needs to be hospitalized. Salmonella infection may spread from the intestines to the bloodstream and then to other places in the body.
- In rare cases, Salmonella infection can cause death unless the person is treated promptly with antibiotics.
Who is more likely to have a severe illness?
- Children younger than 5 years
- Adults older than 65
- People with weakened immune systems
More information about Salmonella and steps people can take to reduce their risk of infection with Salmonella in general can be found on the CDCSalmonella(https://www.cdc.gov/salmonella/general/index.html) website.
Advice to Consumers, Restaurants, and Retailers

Yellow Maradol Papaya: Maradol papayas are a large, oval fruit that weighs 3 or more pounds, with green skins that turn yellow when the fruit is ripe. The flesh inside the fruit is salmon-colored.
CDC recommends that consumers not eat, restaurants not serve, and retailers not sell yellow Maradol papayas until we learn more.
- If you aren’t sure if the papaya you bought is a yellow Maradol papaya, you can ask the place of purchase. Restaurants and retailers can ask their supplier.
- When in doubt, don’t eat, sell, or serve them and throw them out.
- Wash and sanitize countertops as well as drawers or shelves in refrigerators where papayas were stored.
Contact a healthcare provider if you think you got sick from eating contaminated papaya.
- Most people infected with Salmonella develop the following signs and symptoms 12-72 hours after being exposed to the bacteria:
- Diarrhea
- Fever
- Abdominal cramps
Honolulu, Hawaii: 14-day personal disaster kit advised
Saturday, July 22nd, 2017Honolulu-14_DAYS_OF_FOOD_AND_WATER_LOOK_LIKE: Document
Learn – Educate yourself on disasters that can affect you and your Family.
Plan – Create and exercise a Family Disaster Plan. Locate a secondary meeting place and designate an off island contact.
Individual, Family and Business Disaster Planning – Disaster planning is everyone’s business. Carefully review this information and take the time today to discuss preparedness planning with family, friends, neighbors and co-workers.
Video: Learn – Educate yourself on disasters that can affect you and your Family.
Plan – Create and exercise a Family Disaster Plan. Locate a secondary meeting place and designate an off island contact.
Individual, Family and Business Disaster Planning – Disaster planning is everyone’s business. Carefully review this information and take the time today to discuss preparedness planning with family, friends, neighbors and co-workers.
Develop a 14-Day Disaster Supplies Kit
Your disaster supplies kit should contain enough of the following items to last for 14-days minimum:
Water – One gallon of water per person per day for 14 days for drinking and sanitation
Food – Non-perishable food that does not require cooking. Survival foods such as Peanut Butter, Protein Shakes, Dried Fruits, Nuts
Eating Utensils – Plates, mess kits, forks and chop sticks. Don’t forget a non-electric can opener for canned foods
Radio – Battery-powered or hand crank radio with NOAA Weather alert
Light – Flashlight and or a portable fluorescent light
Spare batteries – Check annually
First Aid – Get a good kit and consider enrolling in a certified first aid course
Whistle – Important for signaling for help. A whistle carries much farther than the human voice and uses less energy than yelling
Dust Mask – Helps to filter contaminated air
Sanitation – Moist towelettes, heavy duty garbage bags, hand sanitizer gel, toilet paper, baking soda/kitty litter to absorb orders, gloves and plastic ties for personal sanitation
Tools – Wrench or pliers to turn off utilities, duct tape
Maps – Local area maps
Prescription – Special medications, glasses and medical devices
Pets – Pet food and extra water for your pet
Miscellaneous – Infant Formula, diapers, incontinent supplies, feminine products
Department of Emergency Management City and County of Honolulu Kirk Caldwell, Mayor 650 South King Street ♦ Honolulu, HI 96813 (808) 723-8960 ♦ Fax (808) 524-3439 www.oahuDEM.org email : dem@honolulu.gov
Hawaii is the first state to prepare the public for the possibility of a ballistic missile strike from North Korea.
Saturday, July 22nd, 2017HI-EMA-guidance-analysis-nuclear-detonation-JUN-2017-1: Document

Sirens sound Attack- Warning signal
Emergency Alert System (EAS) advisory
Wireless Emergency Alert (WEA) system advisory
Brilliant white light (flash) is observed
1. If you are indoors, stay indoors well away from windows. 2. If you are outdoors, seek immediate shelter in a building preferably a concrete structure such as a commercial building or parking structure. 3. If you are driving, pull safely to the side of the road and seek shelter in a nearby building or lie flat on the ground. 4. DO NOT look at the flash of light.
• Surviving the immediate effects of a nuclear detonation (blast, shock, thermal radiation, initial nuclear radiation) requires sheltering in resistant structures • You may have only minutes to take protective action – take immediate action without delay • There are no designated blast or fallout shelters in Hawaii • Light generated by the weapon will damage unprotected eyes
1. Remain sheltered until you are told it is safe to leave or two weeks (14 days) have passed, whichever comes first. 2. You may be advised that it is safe to leave your shelter for short periods of time to locate food, water and medical care. 3. Electrical, water and other utilities may be severely disrupted or unavailable.
• Following the detonation, sheltering from radioactive fallout for up to 14 days is critically important • Public may need to briefly leave their shelters to locate essential supplies and equipment • Emergency Management will assess residual radiation levels and advise when sheltering can be discontinued
1. Listen to local AM-FM radio stations for official information. 2. Cell phone, television, radio and internet services will be severely disrupted or unavailable. 3. Small portable walkie-talkies may give you communication with nearby shelters.
• Local AM-FM broadcast radio is most survivable and may be useful in advising the public post-detonation • Other communication technologies may be damaged by weapons effects such as EMP1 • FRS2 and GMRS radios are widely available in the community and may be useful in keeping people in communication with one another.
Comprehensive Preparedness Guide 201: Threat and Hazard Identification and Risk Assessment Guide
Saturday, July 22nd, 2017Document: HomelandSecurity-Haz_Risk_Assess-2013
CPG 201 provides a four-step process for conducting a Threat and Hazard Identification and Risk Assessment. Developing an understanding of its risks from natural, technological, and human-caused threats and hazards, allows a community to make informed decisions about how to manage risk and develop needed capabilities.
FEMA: CPG 101, Developing and Maintaining Emergency Operations Plans, Version 2
Saturday, July 22nd, 2017Guide CPG 101 is designed to help both novice and experienced planners navigate the planning process. Used in its entirety, this Guide provides information and instruction on the fundamentals of planning and their application. Chapters 1 and 2 lay the foundation for planning efforts by providing information on the basics of planning (Chapter 1) and the environment within which planners function (Chapter 2). With an understanding of these fundamentals, the Guide then transitions from theory to practice by discussing the different plan formats and functions (Chapter 3) and moving into an explanation of the planning process (Chapter 4). A detailed checklist, building upon Chapters 3 and 4, is provided in Appendix C. Because Appendix C provides a set of detailed questions to consider throughout the planning process, users are encouraged to copy or remove this checklist and employ it as they work through the planning process in Chapter 4.



