The following information is provided as an informational resource for guidance only. It is not intended as a substitute for professional judgment. These highlights and any hyperlinks may not include all the information needed to use each respective drug or biologic safely and effectively. See full prescribing information (package insert) or IND protocol for each respective drug or biologic, which accompany the product when it is delivered to the treating physician and/or pharmacist.
The Drug Service formulary is subject to change based on current public health needs, updates to treatment guidelines, and/or drug availability. For historical reference, we have included products no longer supplied by the Drug Service.
| Product & Supplier |
Indication & Eligibility |
How Supplied |
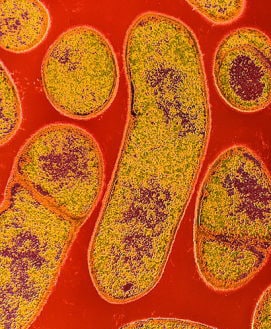
| Anthrax Vaccine Absorbed
(Also known as “AVA”; BioThrax®, Emergent BioSolutions) |
For the active immunization for the prevention of disease caused by Bacillus anthracis, in persons 18 through 65 years of age at high risk for exposure
Because the risk for anthrax infection in the general population is low, routine immunization is not recommended
The safety and efficacy of BioThrax® in a post-exposure setting have not been established. |
Suspension for injection in 5 mL multidose vials, each containing 10 doses |
| Artesunate, intravenous
(Supplied to CDC by the Walter Reed Army Institute of Research) |
For the treatment of severe malaria in patients who require parenteral (IV) therapy
Patient must meet the eligibility criteria in the IND protocol |
110 mg; sterile dry-filled powder with phosphate buffer diluent for reconstitution |
| Benznidazole
(Benznidazol, Manufactured by LAFEPE) |
For the treatment of American trypanosomiasis (Chagas disease)
Patient must meet the eligibility criteria in the IND protocol |
100 mg double-scored tablet
12.5 mg dispersible tablet for pediatric use |
| Botulism Antitoxin Heptavalent (Equine), Types A-G
(Also known as “HBAT”; Manufactured by Cangene Corp. – BAT™) |
For the treatment of symptomatic botulism following documented or suspected exposure to botulinum neurotoxin |
20 mL or 50 mL single-use glass vial
May be received frozen or thawed |
| Diethylcarbamazine
(Also known as “DEC”; Supplied to CDC by the World Health Organization; Manufactured by E.I.P.I.C.O.) |
For the treatment of certain filarial diseases, including lymphatic filariasis caused by infection with Wuchereria bancrofti, Brugia malayi, or Brugia timori; tropical pulmonary eosinophilia; and loiasis
For prophylactic use in persons determined to be at increased risk for Loa loa infection
Patient must meet the eligibility criteria in the IND protocol |
100 mg tablet |
| Diphtheria Antitoxin (Equine)
(Also known as “DAT”; Manufactured by Instituto Butantan) |
For prevention or treatment of actual or suspected cases of diphtheria
Patient must meet the eligibility criteria in the IND protocol |
1 mL single-use ampule containing 10,000 units |
| Eflornithine
(Also known as “DFMO”; Supplied to CDC by the World Health Organization; Manufactured by Sanofi Aventis – Ornidyl®) |
For the treatment of second-stage African trypanosomiasis (sleeping sickness) caused by Trypanosoma brucei gambiense, with involvement of the central nervous system |
20 g/100 mL hypertonic solution for IV infusion
Must be diluted with Sterile Water for Injection before use |
| Melarsoprol
(Supplied to CDC by the World Health Organization; Manufactured by Sanofi Aventis – Arsobal®) |
For the treatment of second-stage African trypanosomiasis (sleeping sickness), with involvement of the central nervous system
Patient must meet the eligibility criteria in the IND protocol |
5 mL glass ampule containing 180 mg/5 mL (36 mg/mL) |
| Nifurtimox
(Supplied to CDC by the World Health Organization; Manufactured by Bayer – Lampit®) |
For the treatment of American trypanosomiasis (Chagas disease)
Patient must meet the eligibility criteria in the IND protocol |
120 mg double-scored tablet |
| Sodium Stibogluconate
(Manufactured by GlaxoSmithKline, UK – Pentostam®) |
For the treatment of leishmaniasis
Patient must meet the eligibility criteria in the IND protocol |
Solution for injection in 100 mL multidose bottle
100 mg pentavalent antimony (Sb) per mL |
| Suramin
(Supplied to CDC by the World Health Organization; Manufactured by Bayer – Germanin) |
For the treatment of first-stage African trypanosomiasis (sleeping sickness) caused by Trypanosoma brucei rhodesiense, without involvement of the central nervous system
Patient must meet the eligibility criteria in the IND protocol |
1 gram of suramin for injection in a 10 mL vial (100 mg/mL solution of suramin sodium)
Must be reconstituted with 10 mL Sterile Water for Injection before use |
| Vaccinia Vaccine
(Also known as the “Smallpox Vaccine”; Manufactured by Sanofi Aventis – ACAM2000®) |
For active immunization against smallpox disease for persons determined to be at high risk for smallpox infection |
Lyophilized powder reconstituted with diluent (provided)
Contains 100 doses per vial |
Top of Page
Anthrax Vaccine Adsorbed
Anthrax Vaccine Adsorbed (AVA) is indicated for the active immunization for the prevention of disease caused by Bacillus anthracis, in persons 18 through 65 years of age at high risk for exposure. The safety and efficacy of AVA in a post-exposure setting have not been established.
CDC provides anthrax vaccine for laboratory workers conducting research under federally funded projects who require preexposure vaccination based on their occupational risk.
Preexposure vaccination is recommended for laboratorians at risk for repeated exposure to fully virulent B. anthracis spores, such as those who 1) work with high concentrations of spores with potential for aerosol production; 2) handle environmental samples that might contain powders and are associated with anthrax investigations; 3) routinely work with pure cultures of B. anthracis; 4) frequently work in spore-contaminated areas after a bioterrorism attack; or 5) work in other settings where repeated exposures to B. anthracis aerosols may occur. Read more[PDF – 36 pages](https://www.cdc.gov/mmwr/pdf/rr/rr5906.pdf).
More Information for Clinicians
CDC’s Anthrax Vaccination Website
Educational Toolkit for Clinicians (from Department of Defense Anthrax Immunization Program)
Vaccine Information Statement (VIS) for Anthrax Vaccine[PDF – 2 pages](https://www.cdc.gov/vaccines/hcp/vis/vis-statements/anthrax.pdf)
Full Prescribing Information for BioThrax®
How to Request
Anthrax vaccine must be administered by or under the supervision of the physician who registers with CDC.
Contact the CDC Drug Service for more information.
Top of Page
Artesunate, Intravenous
Artesunate is in the class of medications known as artemesinins, which are derivatives from the “qinghaosu” or sweet wormwood plant (Artemisia annua). Artesunate is not currently licensed by FDA but is made available in the United States under a CDC-sponsored IND protocol for treatment of documented cases of severe malaria(https://www.cdc.gov/malaria/about/index.html) that require parenteral therapy. Read more(https://www.cdc.gov/malaria/diagnosis_treatment/artesunate.html).
More Information for Clinicians
Diagnostic assistance for malaria is available through DPDx.
How to Request
Clinicians who wish to obtain artesunate for severe malaria should contact the CDC Malaria Hotline at 770-488-7788 (M-F, 8am-4:30pm, Eastern time) or, after hours, the CDC Emergency Operations Center (EOC) at 770-488-7100, and request to speak with a CDC Malaria Branch clinician. A Malaria Branch clinician will provide clinical consultation by telephone and, if indicated, authorize the emergency release of artesunate from one of the CDC Quarantine Stations located in major airports around the nation, ensuring delivery to any location in the United States within hours.
Requests for unapproved uses cannot be granted.
For non-emergency questions related to artesunate IV, contact the CDC Drug Service.
Top of Page
Benznidazole
Benznidazole is a 2-nitroimidazole trypanocidal agent that was introduced in 1971 for the treatment of Trypanosoma cruzi infection—i.e., Chagas disease, also known as American trypanosomiasis(https://www.cdc.gov/parasites/chagas/). Benznidazole is one of two drugs available from CDC for the treatment of Chagas disease (the other is nifurtimox). In the United States, the need to have drugs available for treating Chagas disease has been increasing, largely because of implementation of T. cruzi blood-donor screening in 2007, which has identified chronically infected persons (mainly Latin American immigrants) who might benefit from treatment and has heightened awareness of Chagas disease.
More Information for Clinicians
Evaluation and Treatment of Chagas Disease in the United States: A Systematic Review (JAMA 2007: 298:2171-81)
Screening and Treatment of Chagas Disease in Organ Transplant Recipients in the United States: Recommendations from the Chagas in Transplant Working Group (American Journal of Transplantation, 2011: 672–680)
Diagnostic assistance for American trypanosomiasis is available through DPDx.
How to Request
Contact the CDC Drug Service for more information.
Questions regarding treatment of Chagas disease should be directed to CDC Parasitic Diseases Inquiries (404-718-4745; email chagas@cdc.gov) M-F 7:30am-4pm EST.
For emergencies (for example, acute Chagas disease with severe manifestations, Chagas disease in a newborn, or Chagas disease in an immunocompromised person) outside of regular business hours, call the CDC Emergency Operations Center (770-488-7100) and ask for the person on call for Parasitic Diseases.
Top of Page
Botulism Antitoxin Heptavalent (Equine), Types A-G
Botulism Antitoxin Heptavalent (HBAT) contains equine-derived antibody to the seven known botulinum toxin types (A-G). HBAT is composed of <2% intact immunoglobulin G (IgG) and ≥90% Fab and F(ab’)2 immunoglobulin fragments. These fragments are created by the enzymatic cleavage and removal of Fc immunoglobulin components in a process sometimes referred to as despeciation. HBAT is supplied on an emergency basis for the treatment of persons thought to be suffering from botulism and works by neutralizing unbound toxin molecules. In 2010, HBAT became the only botulism antitoxin available in the United States for naturally occurring non-infant botulism.
It is available only from CDC because of its limited use and its relatively short expiration date. The antitoxin is stored at CDC Quarantine Stations located in major airports around the nation, ensuring delivery to any location in the United States within hours.
BabyBIG® (botulism immune globulin) remains available for infant botulism through the California Infant Botulism Treatment and Prevention Program.
More Information for Clinicians
Clinical Guidance
How to Request
Clinicians who suspect a diagnosis of botulism in a patient should immediately call their state health department’s 24-hour telephone number(https://www.cdc.gov/mmwr/international/relres.html) to maintain effective botulism surveillance and to facilitate rapid detection of outbreaks. The state health department will contact CDC to arrange for a clinical consultation by telephone and, if indicated, release of botulism antitoxin. State health departments requesting botulism antitoxin should contact the CDC Emergency Operations Center (EOC) at 770-488-7100. Read more(https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5232a8.htm).
For non-emergency questions concerning botulism antitoxin, contact the CDC Drug Service.
Top of Page
Diethylcarbamazine (DEC)
DEC is an antihelminthic agent used for treatment of lymphatic filariasis (caused by infection with Wuchereria bancrofti, Brugia malayi, or Brugia timori), tropical pulmonary eosinophilia, and loiasis(https://www.cdc.gov/parasites/loiasis/); DEC also has prophylactic benefit for Loa loa infection. DEC has been used worldwide for more than 50 years. In the past, Wyeth-Ayerst Laboratories made DEC available as a licensed drug; in the late 1990s, because of unavailability of a bulk chemical supplier, Wyeth-Ayerst discontinued distribution of DEC in the United States.
More Information for Clinicians
Diagnostic assistance for filarial diseases is available through DPDx.
How to Request
Contact the CDC Drug Service for more information.
Questions regarding treatment of filarial diseases should be directed to CDC Parasitic Diseases Inquiries (404-718-4745; email parasites@cdc.gov) M-F 7:30am-4pm EST.
After-hours emergencies: 1-770-488-7100
Top of Page
Diphtheria Antitoxin (Equine)
Diphtheria antitoxin (DAT) is used to prevent or treat diphtheria by neutralizing the toxins produced by Corynebacterium diphtheriae. DAT is a sterile, aqueous solution of the refined and concentrated proteins, chiefly globulins, containing antibodies obtained from the serum of horses that have been immunized against diphtheria toxin. DAT is available under an IND protocol sponsored by CDC and is released only for actual or suspected cases of diphtheria(https://www.cdc.gov/diphtheria/about/index.html). The antitoxin is stored at CDC Quarantine Stations located in major airports around the nation, ensuring delivery to any location in the United States within hours.
More Information for Clinicians
CDC’s Vaccine-Related Topics: Diphtheria Antitoxin(https://www.cdc.gov/diphtheria/dat.html)
How to Request
Clinicians who suspect a diagnosis of respiratory diphtheria can obtain DAT by contacting the Emergency Operations Center at 770-488-7100. They will be connected with the diphtheria duty officer, who will provide clinical consultation and, if indicated, initiate the release of diphtheria antitoxin.
For non-emergency questions concerning diphtheria antitoxin, contact the CDC Drug Service.
Top of Page
Eflornithine
Eflornithine is an antitrypanosomal agent that inhibits the enzyme ornithine decarboxylase. Antitrypanosomal treatment is indicated for all persons diagnosed with African trypanosomiasis (sleeping sickness)(https://www.cdc.gov/parasites/sleepingsickness/); the choice of therapy depends on the infecting subspecies of the parasite and on the stage of the infection. Eflornithine is considered the drug of choice for the treatment of second-stage Trypanosoma brucei gambiense (West African) infection, with involvement of the central nervous system. It is not effective against T. b. rhodesiense (East African) infection (see melarsoprol). Although the manufacturer, Aventis, maintains its US licensure, eflornithine is not commercially available in the United States.
More Information for Clinicians
Human African trypanosomiasis, WHO
Diagnostic assistance for African trypanosomiasis is available through DPDx.
How to Request
Contact the CDC Drug Service for more information.
Questions regarding treatment of African trypanosomiasis should be directed to CDC Parasitic Diseases Inquiries (404-718-4745; email parasites@cdc.gov) M-F 7:30am-4pm EST.
For emergencies outside of regular business hours, call the CDC Emergency Operations Center (770-488-7100) and ask for the person on call for Parasitic Diseases.
Top of Page
Melarsoprol
Melarsoprol is an organoarsenic compound with trypanocidal effects that has been used outside the United States since 1949. Antitrypanosomal treatment is indicated for all persons diagnosed with African trypanosomiasis (sleeping sickness)(https://www.cdc.gov/parasites/sleepingsickness/); the choice of therapy depends on the infecting subspecies of the parasite and on the stage of the infection. Melarsoprol is used for the treatment of second-stage infection (involving the central nervous system). It is the only available therapy for second-stage Trypanosoma brucei rhodesiense (East African) infection, whereas eflornithine typically is used for second-stage T. b. gambiense (West African) infection.
More Information for Clinicians
Human African trypanosomiasis, WHO
Diagnostic assistance for African trypanosomiasis is available through DPDx.
How to Request
Contact the CDC Drug Service for more information.
Questions regarding treatment of African trypanosomiasis should be directed to CDC Parasitic Diseases Inquiries (404-718-4745; email parasites@cdc.gov) M-F 7:30am-4pm EST.
For emergencies outside of regular business hours, call the CDC Emergency Operations Center (770-488-7100) and ask for the person on call for Parasitic Diseases.
Top of Page
Nifurtimox
Nifurtimox is a nitrofuran analog that was introduced in 1965 for the treatment of Trypanosoma cruzi infection—i.e., Chagas disease, also known as American trypanosomiasis(https://www.cdc.gov/parasites/chagas/). Nifurtimox is one of two drugs available from CDC for the treatment of Chagas disease (the other is benznidazole). In the United States, the need to have drugs available for treating Chagas disease has been increasing, largely because of implementation of T. cruzi blood-donor screening in 2007, which has identified chronically infected persons (mainly Latin American immigrants) who might benefit from treatment and has heightened awareness of Chagas disease.
More Information for Clinicians
Evaluation and Treatment of Chagas Disease in the United States: A Systematic Review (JAMA 2007: 298:2171-81)
Screening and Treatment of Chagas Disease in Organ Transplant Recipients in the United States: Recommendations from the Chagas in Transplant Working Group (American Journal of Transplantation, 2011: 672–680)
Diagnostic assistance for American trypanosomiasis is available through DPDx.
How to Request
Contact the CDC Drug Service for more information.
Questions regarding treatment of Chagas disease should be directed to CDC Parasitic Diseases Inquiries (404-718-4745; email chagas@cdc.gov) M-F 7:30am-4pm EST.
For emergencies (for example, acute Chagas disease with severe manifestations, Chagas disease in a newborn, or Chagas disease in an immunocompromised person) outside of regular business hours, call the CDC Emergency Operations Center (770-488-7100) and ask for the person on call for Parasitic Diseases.
Top of Page
Sodium Stibogluconate
Sodium stibogluconate (Pentostam®) is a pentavalent antimony compound used for treatment of leishmaniasis(https://www.cdc.gov/parasites/leishmaniasis). The three main clinical syndromes in humans are visceral, cutaneous, and mucosal leishmaniasis. Pentostam is a well-established antileishmanial agent that has been used in many countries of the world for more than half a century.
More Information for Clinicians
Recommendations for Treating Leishmaniasis with Sodium Stibogluconate (Pentostam) and Review of Pertinent Clinical Studies (Am J Trop Med 1992:46(3):296-306)[PDF, 11 pages]
Diagnostic assistance for leishmaniasis is available through DPDx.
Practical Guide for Laboratory Diagnosis of Leishmaniasis[PDF, 4 pages](https://www.cdc.gov/parasites/leishmaniasis/resources/pdf/cdc_diagnosis_guide_leishmaniasis.pdf)
How to Request
Contact the CDC Drug Service for more information.
Questions regarding treatment of leishmaniasis should be directed to CDC Parasitic Diseases Inquiries (404-718-4745; email parasites@cdc.gov) M-F 7:30am-4pm EST.
After-hours emergencies: 1-770-488-7100
Top of Page
Suramin
Suramin is a negatively charged, high-molecular-weight sulfated naphthylamine. It was introduced in the 1920s for the treatment of African trypanosomiasis (sleeping sickness)(https://www.cdc.gov/parasites/sleepingsickness/). Suramin generally is considered the drug of choice for first-stage Trypanosoma brucei rhodesiense (East African) infection, without involvement of the central nervous system. Pentamidine typically is used for first-stage T. b. gambiense (West African) infection.
More Information for Clinicians
Human African trypanosomiasis, WHO
Diagnostic assistance for African trypanosomiasis is available through DPDx.
How to Request
Contact the CDC Drug Service for more information.
Questions regarding treatment of African trypanosomiasis should be directed to CDC Parasitic Diseases Inquiries (404-718-4745; email parasites@cdc.gov) M-F 7:30am-4pm EST.
For emergencies outside of regular business hours, call the CDC Emergency Operations Center (770-488-7100) and ask for the person on call for Parasitic Diseases.
Top of Page
Vaccinia Vaccine, “Smallpox Vaccine”
Smallpox vaccine is made of live vaccinia virus derived from plaque purification cloning of Dryvax® (calf lymph vaccine, New York City Board of Health Strain) and grown in African Green Monkey kidney (Vero) cells and tested to be free of adventitious agents. It contains approximately 2.5 – 12.5 x 105 plaque-forming units per dose.
Smallpox was declared globally eradicated in 1980. In 1982, Wyeth Laboratories, the only active manufacturer of licensed vaccinia vaccine in the United States, discontinued production; and, in 1983, distribution to the civilian population was discontinued. Since January 1982, smallpox vaccination has not been required for international travelers, and International Certificates of Vaccination no longer include smallpox vaccination. ACAM2000® is a new-generation smallpox vaccine that was licensed in 2010 for use as a medical countermeasure held by the Strategic National Stockpile.
CDC recommends vaccinia vaccine for laboratory workers who directly handle a) cultures or b) animals contaminated or infected with nonhighly attenuated vaccinia virus, recombinant vaccinia viruses derived from nonhighly attenuated vaccinia strains, or other orthopoxviruses that infect humans (e.g., monkeypox, cowpox, vaccinia, and variola). Other health-care workers (e.g., physicians and nurses) whose contact with nonhighly attenuated vaccinia viruses is limited to contaminated materials (e.g., dressings) and who adhere to appropriate infection control measures are at lower risk for inadvertent infection than laboratory workers. However, because a theoretical risk for infection exists, vaccination can be offered to this group. Read more[PDF – 930KB](https://www.cdc.gov/mmwr/pdf/rr/rr5010.pdf).
More Information for Clinicians
Full Prescribing Information for ACAM2000®[PDF – 11 pages]
ACAM2000® Medication Guide[PDF – 6 pages]
MMWR Notice to Readers: Newly Licensed Smallpox Vaccine to Replace Old Smallpox Vaccine(https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5708a6.htm)
CDC’s Vaccine-Related Topics: Smallpox Vaccine
How to Request
Smallpox vaccine must be administered by or under the supervision of the physician who registers with CDC.
Ancillary supplies, such as bifurcated needles (for administration) and 1 mL tuberculin syringes with 25 gauge x 5/8″ needles (for reconstitution), are supplied with the vaccine.
Contact the CDC Drug Service for more information.
Requests for unapproved uses cannot be granted.
Top of Page
Products No Longer Supplied by Drug Service*
Botulinum Toxoid
Pentavalent (ABCDE) botulinum toxoid is a combination of aluminum phosphate-adsorbed toxoid derived from formalin-inactivated types A, B, C, D, and E botulinum toxins, with formaldehyde and thimerosal used as preservatives. Botulinum toxoid was distributed by CDC under an IND protocol for at-risk persons who were actively working or expected to be working with cultures of Clostridium botulinum or the toxins; in 2011, CDC discontinued its program to supply this vaccine. Read more(https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6042a3.htm).
Botulinum Antitoxin Types AB & E
In March 2010, CDC announced the availability of a new heptavalent botulinum antitoxin (HBAT, Cangene Corporation). HBAT replaced the licensed bivalent botulinum antitoxin AB and an investigational monovalent botulinum antitoxin E (BAT-AB and BAT-E, Sanofi Pasteur), becoming the only botulinum antitoxin available in the United States for naturally occurring non-infant botulism. Read more(https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5910a4.htm).
Vaccinia Immune Globulin (VIG)
Vaccinia immune globulin (VIG) is released from the CDC Strategic National Stockpile, if indicated, for the treatment of complications associated with vaccinia vaccination. Clinicians wishing to obtain VIG should contact the Emergency Operations Center (EOC) at 770-488-7100. They will be connected with CDC medical staff who can assist them in the diagnosis and management of patients with suspected complications of vaccinia vaccination.
*this list is not all-inclusive
Use of trade names is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services.