Archive for the ‘Plague’ Category
First Plague Case in New Mexico in 2017
Thursday, June 8th, 2017Plague Case in Santa Fe County Man
First Case in New Mexico in 2017
The New Mexico Department of Health (NMDOH) has confirmed a case of plague in a 63-year-old man from Santa Fe County who is currently hospitalized. Confirmatory testing was conducted at the NMDOH Scientific Laboratory Division. This is the first human case of plague in New Mexico this year.
NMDOH is conducting an environmental investigation at the man’s home to look for ongoing risk and to ensure the health of the immediate family and neighbors. Additionally, staff are going door-to-door to neighbors near the patient’s home to inform them about plague found in the area and educate them on reducing their risk.
Plague is a bacterial disease of rodents and is generally transmitted to humans through the bites of infected fleas, but can also be transmitted by direct contact with infected animals, including rodents, wildlife and pets. To date, there have been ten dogs and five cats with confirmed plague in New Mexico in 2017. The animals come from Los Alamos, Santa Fe, Bernalillo, Sandoval, Torrance, and Taos counties.
“Plague activity has been widespread in northcentral New Mexico this spring,” said Dr. Paul Ettestad, public health veterinarian for the Department of Health. “Sick or dead rodents and rabbits are being reported from different areas in the state so it is very important to take precautions to avoid rodents and their fleas which can expose you to plague. Pets that are allowed to roam and hunt can bring plague-infected fleas from dead rodents back into the home, putting you and your children at risk.”
To prevent plague, the Department of Health recommends residents:
- Avoid sick or dead rodents and rabbits, and their nests and burrows.
- Keep pets from roaming and hunting.
- Provide safe and effective flea control for pets; if possible, talk with a veterinarian about using an appropriate flea control product on pets as not all products are safe for cats, dogs, or children.
Clean up areas near the house where rodents could live, such as woodpiles, brush piles, junk and abandoned vehicles. - Sick pets should be examined promptly by a veterinarian.
- See a healthcare provider about any unexplained illness involving a sudden and severe fever.
- Put hay, wood, and compost piles as far as possible from the home.
- Don’t leave your pet’s food and water where rodents can get to it.
Symptoms of plague in humans include sudden onset of fever, chills, headache, and weakness. In most cases, there is a painful swelling of the lymph node in the groin, armpit or neck areas which is a sign of the most common form of plague. There are two other forms of plague seen less commonly in which people can have fever, chills, weakness and abdominal pain indicating the type of plague that is in their bloodstream, and sometimes shortness of breath, chest pain and cough indicating pneumonia that can be associated with plague. Plague signs in cats and dogs are fever, lethargy and loss of appetite. There may be a swelling in the lymph node under the jaw of pets. Prompt diagnosis and appropriate antibiotic treatment can greatly reduce the risk of death in people. Healthcare providers who suspect a patient may have plague should promptly report it to the Department of Health on-call epidemiologist using the Reporting & Surveillance hotline at 505-827-0006.
There were four human plague cases identified in New Mexico in 2016. All four cases recovered.
For more information, please visit the Plague section of our website.
5 cases of culture-confirmed human plague treated successfully with oral ciprofloxacin
Thursday, February 2nd, 2017Abstract: “The US Food and Drug Administration recently approved ciprofloxacin for treatment of plague (Yersina pestis infection) based on animal studies. Published evidence of efficacy in humans is sparse. We report 5 cases of culture-confirmed human plague treated successfully with oral ciprofloxacin, including 1 case of pneumonic plague.”
Apangu T, Griffith K, Abaru J, Candini G, Apio H, Okoth F, et al. Successful treatment of human plague with oral ciprofloxacin. Emerg Infect Dis. 2017 Mar [date cited]. http://dx.doi.org/10.3201/eid2303.161212
Demographic and clinical characteristics of 5 patients with culture-confirmed plague (Yersina pestis infection) who were treated successfully with oral ciprofloxacin, Uganda, 2011–2014
| Patient no. | Age, y/sex | Length of illness, d* | Symptoms | Laboratory evidence | Ciprofloxacin dose, mg† |
|---|---|---|---|---|---|
| 1 | 10/F | 7 | Fever, left axillary bubo | Bubo, blood cultures positive | 250 |
| 2 | 52/F | 4 | Fever, right axillary bubo | Bubo, blood cultures positive | 650 |
| 3 | 27/F | 1 | Fever, left inguinal bubo | Bubo, blood cultures positive | 750 |
| 4 | 36/M | 1 | Fever, left axillary bubo | Blood culture positive | 625 |
| 5 | 13/M | 6 | Fever, chest pain, cough, blood-tinged sputum | Sputum culture positive, blood culture negative | 375 |
*At time treatment was sought.
†Orally, twice daily; ≈15 mg/kg bodyweight with a maximum of 750 mg.
Pneumonic plague persists as a threat in Madagascar, where poor healthcare systems and traditional burial practices promote these outbreaks.
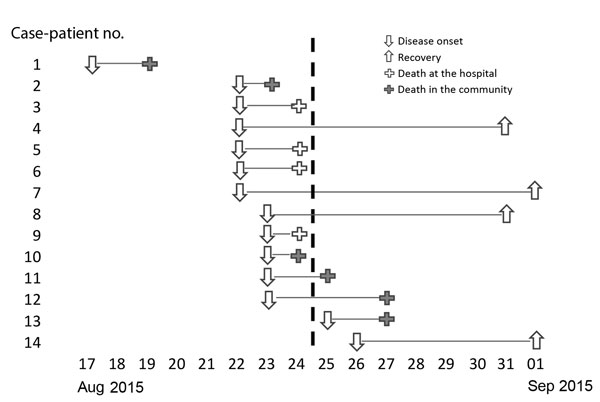
Thursday, February 2nd, 2017Abstract: “During a pneumonic plague outbreak in Moramanga, Madagascar, we identified 4 confirmed, 1 presumptive, and 9 suspected plague case-patients. Human-to-human transmission among close contacts was high (reproductive number 1.44) and the case fatality rate was 71%. Phylogenetic analysis showed that the Yersinia pestis isolates belonged to group q3, different from the previous outbreak.”
Ramasindrazana B, Andrianaivoarimanana V, Rakotondramanga JM, Birdsell DN, Ratsitorahina M, Rajerison M. Pneumonic plague transmission, Moramanga, Madagascar, 2015. Emerg Infect Dis. 2017 Mar [date cited]. http://dx.doi.org/10.3201/eid2303.161406
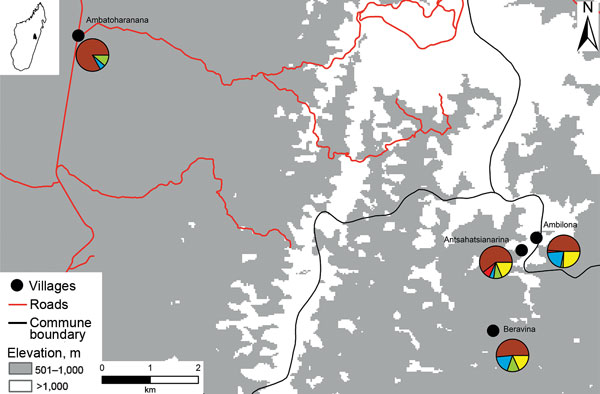
Map of pneumonic plague outbreak (n = 14) in the commune of Ampasipotsy Gara in Moramanga, Madagascar, 2015. The index case-patient (case-patient 1) was infected with Yersinia pestis at Antsahatsianarina and spread the bacterium to Beravina (burial site of case-patient 1), Ambilona (case-patient 10’s home), and Ambatoharanana (burial site of case-patient 2 and home of case-patient 14). Each pie chart indicates the proportions of plague cases (red), seropositive contacts (blue), seronegative contacts (green), unsampled contacts (yellow), and noncontacts (brown) among the total inhabitants of each site.
The mountainous area of Befotaka in southeastern Madagascar has seen 68 cases — of which 27 have died — since the end of last year.
Monday, January 23rd, 2017There has been a rise in the number of human plague cases globally resulting in the categorisation of Yersinia pestis, the aetiological agent of the highly fatal pneumonic plague, as a re-emerging pathogen by the WHO.
Wednesday, January 18th, 2017“….The progression of pneumonic plague is very rapid after first appearance of the symptoms in humans, and the case fatality rate approaches 100%, if the antimicrobial treatment is delayed. Unfortunately, antibiotic-resistant Y. pestis strains have been isolated from plague patients and/or engineered for bioweaponization, which is concerning as Y. pestis is classified by the Centers for Disease Control and Prevention (CDC) as a Tier-1 select agent. The optimal strategy for protection against this deadly disease would be through vaccination; however, there are currently no Food and Drug Administration (FDA)-licensed plague vaccines available in the United States.…”

University of Texas Medical Branch at Galveston have developed 3 new possible vaccines against the plague.
Saturday, January 14th, 2017Immunisation of two rodent species with new live-attenuated mutants of Yersinia pestis CO92 induces protective long-term humoral- and cell-mediated immunity against pneumonic plague; Bethany L Tiner, Jian Sha, Yingzi Cong, et al. Vaccines 1, Article number: 16020 (2016); doi:10.1038/npjvaccines.2016.20
“…It is crucial that a potential vaccine candidate(s) demonstrates long-term immune responses and protection. This is the first study to examine several components of the immune response generated after immunisation of mice and rats with the above three live-attenuated mutants over a period of 3–4 months……Overall, all three live-attenuated mutants stimulated long-lasting T cell-mediated immune responses capable of protecting mice from developing subsequent pneumonic plague….Most importantly, all three live-attenuated mutants stimulated both long-term humoral- and cell-mediated immune responses, which protected mice against exposure to highly lethal pneumonic challenge….”
Madagascar is battling an outbreak of 62 cases of bubonic and pneumonic plague, including 26 deaths.
Wednesday, January 11th, 2017On 6 December 2016, the Ministry of Health (MoH) in Madagascar alerted WHO of a suspected plague outbreak in Befotaka district, Atsimo Atsinanana region in the south-eastern part of the country. The district is outside the area known to be endemic area in Madagascar. No plague cases have been reported in this area since 1950.
As of 27 December 2016, 62 cases (6 confirmed, 5 probable, 51 suspected) including 26 deaths (case fatality rate of 42%) have been reported in two adjacent districts in two neighbouring regions of the country. 28 cases, including 10 deaths have been reported from Befotaka District in Atsimo-Atsinanana Region and 34 cases including 16 deaths have been reported from Iakora district in Ihorombe Region.
Of the 11 samples tested, 5 were positive for plague on rapid diagnostic test and 6 are now confirmed at Institut Pasteur laboratory. Of the total reported cases, 5 are classified as pneumonic plague cases and the remaining as bubonic plague.
Retrospective investigations carried out in those two districts showed that it is possible that the outbreak might have started in mid-August 2016. The investigation in neighbouring villages is still ongoing. On 29 December, an investigation carried out within 25 km of the initial foci in Befotaka district has reported three deaths and is being investigated further for possible linkage to the outbreak.
The affected zone is located in a very remote and hard to reach and highly insecure area (classified as red zone due to local banditry). Despite arrangements made with the local authorities, insecurity slows down the investigations and response activities. In addition, a helicopter has been made available but its use has been limited due to bad weather and financial limitations.
Public Health Response
On 6 December, a 15 member multidisciplinary team from MoH, Institute Pasteur including public health professional, epidemiologist, entomologist and laboratory professional visited the affected area for epidemiological investigation and response activities.
Key response activities already implemented include:
- Epidemiological investigations including active case finding and rapid diagnostic testing
- Training of community health workers on community-based surveillance and early detection of cases
- Clinical Management of suspected cases
- Identification, follow up and chemoprophylaxis of contacts
- Vector and reservoir control through the use of Kartman boxes
- Sensitization of the population
- Strengthening the community based surveillance
- Free treatment of other diagnosed disease such as malaria
- Strengthening early detection in neighbouring districts
- Laboratory confirmation
WHO Risk Assessment
Based on the available information to date, the risk of international spread appears unlikely, especially as it is occurring in very remote area. However, the difficulty to reach the affected area hampered prompt investigation and therefore at this stage the real magnitude of the outbreak is still to be defined and the risk of further spread in the area and sustained transmission cannot be formally ruled out. WHO continues supporting ongoing investigation and response activities.
WHO Advice
Further ecological investigations will be needed to understand the occurrence of a plague outbreak in an area which has not reported any cases of plague since 1950 in order to adapt long term surveillance and control measures.
The outbreak impacts rural communities which have already suffered from remoteness and inadequate access to health services. Staff from MoH are supported by Pasteur Institute of Madagascar, who are all experienced on control measures. However, local conditions make their implementation complex.
Due to the remoteness of the affected area and the conditions for getting infected by the disease, the current outbreak does not represent a significant risk for travellers.
In August 2015, plague was diagnosed for 2 persons (septicemic and bubonic) who had visited Yosemite National Park in California, USA.
Saturday, November 19th, 2016

A person wearing a hat, a mask suggestive of a bird beak, goggles or glasses, and a long gown. The clothing identifies the person as a “plague doctor” and is intended as protection. Descriptions indicate that the gown was made from heavy fabric or leather and was usually waxed. The beak contained pungent substances like herbs or perfumes, thought at the time to purify the air and helpful in relieving the stench. The person also carries a pointer or rod to keep patients at a distance. (Library of Medicine)
A ten-year old boy in Siberia’s Altai Republic has contracted bubonic plague
Thursday, July 14th, 2016“…..According to the World Health Organization, more than 13,000 people contracted bubonic plague in Asia, Africa and America between 2004 and 2013. Roughly 900 of them died from the disease…..”

** Worldwide, between 1 January 2010 and 31 December 2015, 3248 cases of plague in humans were reported, resulting in 584 deaths.
Monday, February 29th, 2016
Weekly epidemiological record
26 FEBRUARY 2016, 91th YEAR
No 8, 2016, 91, 89–104
http://www.who.int/wer




