Archive for the ‘Yellow Fever’ Category
4th case of Yellow Fever reported in Europeans who had recently traveled to South America in the past 8 months.
Thursday, March 16th, 2017A travel-associated case of yellow fever has been reported by the Netherlands in March 2017 after travel to Suriname. During the past eight months, four travel-associated cases of yellow fever have been identified among EU travellers returning from South America. This represents a significant increase on four travel-associated cases of yellow fever among EU travellers during the last 27 years (1999 to July 2016).
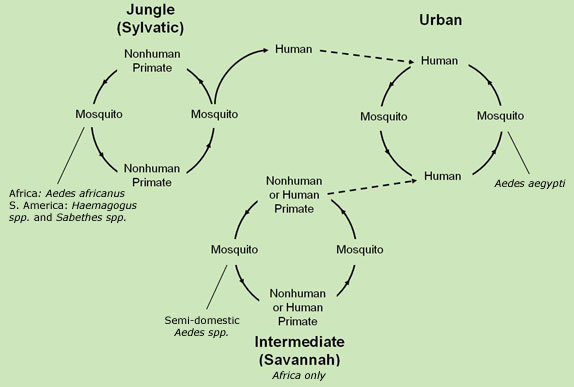
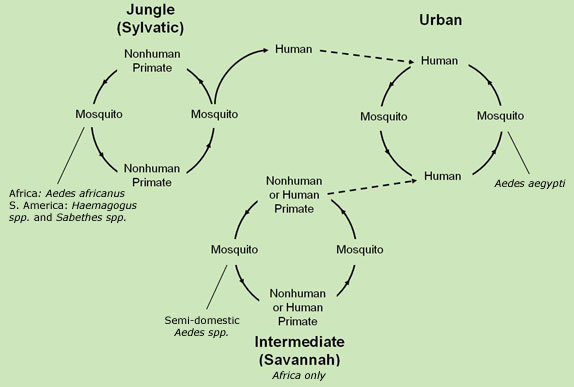
Brazil has been experiencing a yellow fever outbreak since January 2017 and travel recommendations have been updated accordingly [1,2]. Therefore, EU travellers travelling to areas at risk of yellow fever in South America should be informed of the potential exposure to yellow fever virus and an individual risk benefit analysis should be conducted during pre-travel medical consultation. The ongoing yellow fever outbreak in Brazil should be carefully monitored, as the establishment of an urban cycle of yellow fever would have the potential to rapidly affect a significant number of people. The risk of introduction and further transmission of the yellow fever virus in the EU is currently considered very low.
Advice to travellers EU citizens who travel to, or live in areas where there is evidence of periodic or persistent yellow fever virus transmission, especially those in outbreak-affected regions, are advised to:
• Be aware of the risk of yellow fever in endemic areas throughout South America, including recently affected States in Brazil. WHO publishes a list of countries, territories and areas with yellow fever vaccination requirements and recommendations [1-3].
• Check vaccination status and get vaccinated if necessary. Vaccination against yellow fever is recommended from nine months of age for people visiting or living in yellow fever risk areas. An individual risk benefit analysis should be conducted prior to vaccination, taking into account the period, destination, duration of travel and the likelihood of exposure to mosquitoes (e.g. rural areas, forests) as well as individual risk factors for adverse events following yellow fever vaccination.
• Take measures to prevent mosquito bites indoors and outdoors, especially between sunrise and sunset when Aedes and sylvatic yellow fever mosquito vectors are most active [4]. These measures include: − the use of mosquito repellent in accordance with the instructions indicated on the product label; − wearing long-sleeved shirts and long trousers; − sleeping or resting in screened/air-conditioned rooms, or using mosquito nets at night and during the day.
Advice to health professionals: Physicians, health professionals and travel health clinics should be provided with or have access to regularly updated information about areas with ongoing yellow fever transmission and should consider yellow fever in the differential diagnoses for illnesses in relation to travellers returning from affected areas. To reduce the risk of adverse events following immunisation, healthcare practitioners should be aware of contraindications and comply with the manufacturers’ precautionary advice before administering yellow fever vaccine [5].

AGS-v: An investigational vaccine that triggers an immune response to mosquito saliva rather than to a specific virus or parasite carried by mosquitoes
Wednesday, February 22nd, 2017The National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health (NIH), has launched a Phase 1 clinical trial to test an investigational vaccine intended to provide broad protection against a range of mosquito-transmitted diseases, such as Zika, malaria, West Nile fever and dengue fever, and to hinder the ability of mosquitoes to transmit such infections. The study, which is being conducted at the NIH Clinical Center in Bethesda, Maryland, will examine the experimental vaccine’s safety and ability to generate an immune response.

The investigational vaccine, called AGS-v, was developed by the London-based pharmaceutical company SEEK, which has since formed a joint venture with hVIVO in London. The consulting group Halloran has provided regulatory advice to both companies.
Unlike other vaccines targeting specific mosquito-borne diseases, the AGS-v candidate is designed to trigger an immune response to mosquito saliva rather than to a specific virus or parasite carried by mosquitoes. The test vaccine contains four synthetic proteins from mosquito salivary glands. The proteins are designed to induce antibodies in a vaccinated individual and to cause a modified allergic response that can prevent infection when a person is bitten by a disease-carrying mosquito.
“Mosquitoes cause more human disease and death than any other animal,” said NIAID Director Anthony S. Fauci, M.D. “A single vaccine capable of protecting against the scourge of mosquito-borne diseases is a novel concept that, if proven successful, would be a monumental public health advance.”
Led by Matthew J. Memoli, M.D., director of the Clinical Studies Unit in NIAID’s Laboratory of Infectious Diseases, the clinical trial is expected to enroll up to 60 healthy adults ages 18 to 50 years. Participants will be randomly assigned to receive one of three vaccine regimens. The first group will receive two injections of the AGS-v vaccine, 21 days apart. The second group will receive two injections of AGS-v combined with an adjuvant, 21 days apart. The adjuvant is an oil and water mixture commonly added to vaccines to enhance immune responses. The third group will receive two placebo injections of sterile water 21 days apart. Neither the study investigators nor the participants will know who is assigned to each group.
Participants will be asked to return to the clinic twice between vaccinations and twice after the second vaccination to undergo a physical exam and to provide blood samples. Study investigators will examine the blood samples to measure levels of antibodies triggered by vaccination.
Each participant also will return to the Clinical Center approximately 21 days after completing the vaccination schedule to undergo a controlled exposure to biting mosquitoes. The mosquitoes will not be carrying viruses or parasites, so the participants are not at risk of becoming infected with a mosquito-borne disease. Five to 10 female Aedes aegypti mosquitoes from the insectary in NIAID’s Laboratory of Malaria and Vector Research will be put in a feeding device that will be placed on each participant’s arm for 20 minutes. The mosquitoes will bite the participants’ arms through the netting on the feeding devices.
Afterward, investigators will take blood samples from each participant at various time points to see if participants experience a modified response to the mosquito bites as a result of AGS-v vaccination.
Investigators also will examine the mosquitoes after the feeding to assess any changes to their life cycle. Scientists suspect that the mosquitoes who take a blood meal from ASG-v-vaccinated participants may have altered behavior that could lead to early death or a reduced ability to reproduce. This would indicate that the experimental vaccine could also hinder disease transmission by controlling the mosquito population.
All participants will be asked to return to the clinic for follow-up visits every 60 days for five months following the mosquito feeding. A final clinic visit to assess long-term safety will take place approximately 10 months after the mosquito feeding. Throughout the trial, an independent Data and Safety Monitoring Board will review study data to evaluate participant safety and the overall conduct of the study. A medical monitor from NIAID’s Office of Clinical Research Policy and Regulatory Operations will also perform routine safety assessments.
The study is expected to be completed by summer 2018. For more information about the trial, see ClinicalTrials.gov using the trial identifier NCT03055000 (link is external).
Brazil: The number of confirmed cases of Yellow Fever in Minas Gerais rose to 109
Friday, February 3rd, 2017
The number of suspected yellow fever cases in Brazil is climbing quickly, with 421 suspected infections and two more states reporting cases.
Wednesday, January 25th, 2017Yellow fever – Brazil
Wednesday, January 18th, 2017On 6 January 2017, the Brazil Ministry of Health (MoH) reported 12 suspected cases of yellow fever from six municipalities in the state of Minas Gerais.
On the same day, the Brazil IHR National Focal Point (NFP) informed PAHO/WHO that the 12 cases are male, residing in rural areas, and have an average age of approximately 37 years (range: 7–53 years). The first of these cases had onset of symptoms on 18 December 2016. Samples from the cases were sent to the State Reference Laboratory (the Ezequiel Dias Foundation) for differential diagnosis, including dengue, hantavirus, leptospirosis, malaria, Rocky Mountain spotted fever, and viral hepatitis (A, B, C, D, and E). Results are pending.
On 12 January, the Brazil IHR NFP provided an update on the event informing that a total of 110 suspected cases, including 30 deaths, had been reported from 15 municipalities of Minas Gerais: Ladainha (31 cases, 11 deaths), Caratinga (20 cases, 1 death), Imbe de Minas (14 cases, 1 death), Piedade de Caratinga (12 cases, 4 deaths), Poté (6 cases, 3 deaths), Ubaporanga (6 cases, 2 deaths), Itambacuri (5 cases, 3 deaths), Ipanema (4 cases, 1 death), Malacacheta (4 cases, 2 deaths), Entre Folhas (2 cases), Frei Gaspar (1 case), Inhapim (2 cases), São Domingos das Dores (1 case), São Sebastião do Maranhão (1 fatal case), and Setubinha (1 fatal case). Serological tests for 19 suspected cases were positive for yellow fever. Among them, 10 deaths (CFR: 53%) were reported. The report also confirms that there had been epizootics in 13 municipalities of Minas Gerais. Six of these 13 municipalities have not so far reported human cases of yellow fever: Agua Boa, Durande, Ipatinga, Sao Pedro do Sacui, Simonesia, and Teófilo Otoni.
Public health response
Health authorities at the federal, state, and municipal levels are implementing several measures to respond to the outbreak:
- The MoH has deployed technical teams to the state of Minas Gerais to assist the state and municipal secretary of health with surveillance and outbreak investigation, vector control, and coordination of health care services;
- A house-to-house immunization campaign is being conducted in the rural areas of affected municipalities;
- Preparedness activities are being conducted in states bordering Minas Gerais, for a potential introduction of yellow fever;
- The local press is working together with the MoH to keep the public constantly informed on the situation.
WHO risk assessment
Yellow fever outbreak has previously been detected in Minas Gerais. The most recent outbreak occurred in 2002–2003, when 63 confirmed cases, including 23 deaths (CFR: 37%), were detected.
The current yellow fever outbreak is taking place in an area with relatively low vaccination coverage, which could favor the rapid spread of the disease. The concern is that transmission may extend to areas located in proximity of Minas Gerais, such as the state of Espírito Santo and the south of Bahia, which have favorable ecosystems for the transmission of the virus. These areas were previously considered to be at low risk of transmission and, consequently, yellow fever vaccination was not recommended. The introduction of the virus in these areas could potentially trigger large epidemics of yellow fever. There is also a risk that infected humans may travel to affected areas, within or outside of Brazil, where the Aedes mosquitoes are present and initiate local cycles of human-to-human transmission. Response efforts are further complicated by the fact that it is occurring in the context of concomitant outbreaks of Zika virus, chikungunya and dengue.
WHO continues to monitor the epidemiological situation and conduct risk assessment based on the latest available information.
WHO advice
Yellow fever can easily be prevented through immunization provided that vaccination is administered at least 10 days before travel. WHO, therefore, urges Members States especially those where the establishment of a local cycle of transmission is possible (i.e. where the competent vector is present) to strengthen the control of immunisation status of travellers to all potentially endemic areas.
WHO does not recommend any restriction of travel and trade to Brazil based on the current information available.
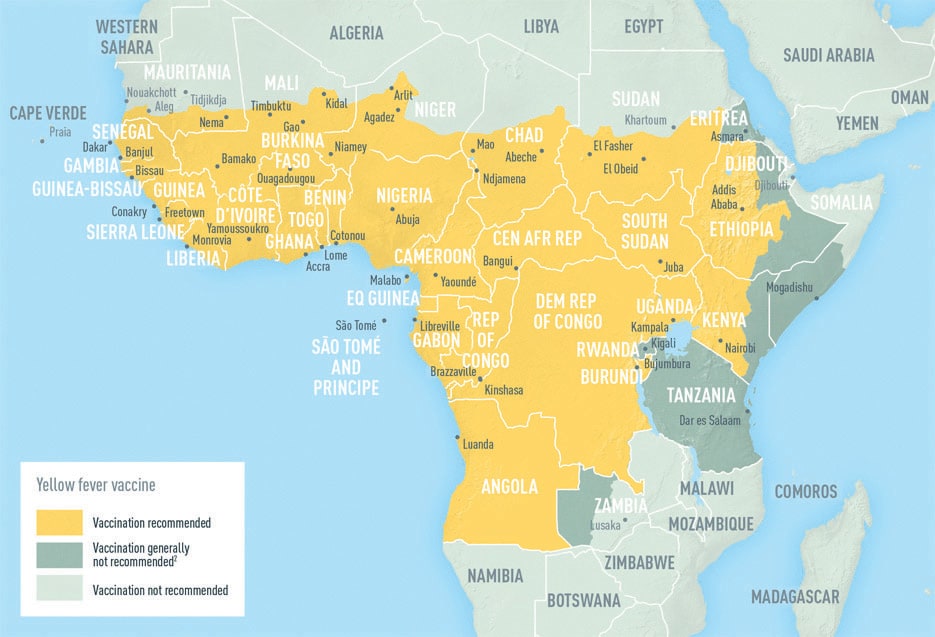
One of the largest emergency vaccination campaigns ever attempted in Africa will start in Angola and the Democratic Republic of Congo this week as WHO and partners work to curb a yellow fever outbreak that has killed more than 400 people and sickened thousands more.
Wednesday, August 17th, 2016CDC
Symptoms
- The majority of persons infected with yellow fever virus have no illness or only mild illness.
- In persons who develop symptoms, the incubation period (time from infection until illness) is typically 3–6 days.
- The initial symptoms include sudden onset of fever, chills, severe headache, back pain, general body aches, nausea, and vomiting, fatigue, and weakness. Most persons improve after the initial presentation.
- After a brief remission of hours to a day, roughly 15% of cases progress to develop a more severe form of the disease. The severe form is characterized by high fever, jaundice, bleeding, and eventually shock and failure of multiple organs.
Treatment
- No specific treatments have been found to benefit patients with yellow fever. Whenever possible, yellow fever patients should be hospitalized for supportive care and close observation.
- Treatment is symptomatic. Rest, fluids, and use of pain relievers and medication to reduce fever may relieve symptoms of aching and fever.
- Care should be taken to avoid certain medications, such as aspirin or other nonsteroidal anti-inflammatory drugs (e.g. ibuprofen, naproxen), which may increase the risk of bleeding.
- Yellow fever patients should be protected from further mosquito exposure (staying indoors and/or under a mosquito net) for up to 5 days after the onset of fever. This way, yellow fever virus in their bloodstream will be unavailable to uninfected mosquitoes, thus breaking the transmission cycle and reducing risk to the persons around them.
Outcome
- The majority of infected persons will be asymptomatic or have mild disease with complete recovery.
- In persons who become symptomatic but recover, weakness and fatigue may last several months.
- Among those who develop severe disease, 20–50% may die.
- Those who recover from yellow fever generally have lasting immunity against subsequent infection.
Since December 2015, Angola has reported 3,867 yellow fever cases, 879 of them confirmed & as of Aug 8 the DRC had reported 2,269 cases, 74 of them confirmed.
Sunday, August 14th, 2016Yellow Fever in Africa: A senior outbreak expert at the WHO acknowledged their response had “lagged” for months.
Tuesday, August 9th, 2016“….Much like its fumbled response to the 2014 Ebola outbreak in West Africa, the UN agency’s efforts to stop yellow fever have been undermined by chronic mismanagement, according to internal UN emails and documents obtained by The Associated Press…..”
YF Update
Saturday, July 30th, 2016Angola: 3748 suspected cases
In Angola, as of 21 July 2016 a total of 3748 suspected cases have been reported, of which 879 are confirmed. The total number of reported deaths is 364, of which 119 were reported among confirmed cases. Suspected cases have been reported in all 18 provinces and confirmed cases have been reported in 16 of 18 provinces and 80 of 125 reporting districts.
Mass reactive vaccination campaigns first began in Luanda and have now expanded to cover most of the other affected parts of Angola. Recently, the campaigns have focused on border areas. All districts continued with house to house immunization campaigns and routine vaccination.
Democratic Republic of the Congo: 1907 suspected cases
According to the latest confirmed information, DRC has reported 1907 suspected cases (as of 20 July) and 68 confirmed cases (as of 24 June) including 95 reported deaths (Table 1). Cases have been reported in 22 health zones in five of 26 provinces. Of the 68 confirmed cases, 59 were imported from Angola, two are sylvatic (not related to the outbreak) and seven are autochthonous.
The recent technical difficulties at the national laboratory in the Democratic Republic of The Congo (DRC) have been resolved and the laboratory confirmation of yellow fever cases in DRC has resumed. According to the preliminary results of tests performed on a backlog samples, seven new patients have tested positive for yellow fever. Additional investigations to determine the definitive status of these cases are ongoing. Until these investigations are completed, the official case count in DRC remains unchanged.
In DRC, surveillance efforts have increased and vaccination campaigns have centred on affected health zones in Kinshasa and Kongo Central and Kwango. Reactive vaccination campaigns started on 20 July in Kisenso health zone in Kinshasa province and in Kahemba, Kajiji and Kisandji health zones in Kwango province.
The risk of spread
Seven countries (Brazil, Chad, Colombia, Ghana, Guinea, Peru and Uganda) have reported yellow fever outbreaks or sporadic cases not linked to the Angolan outbreak.
An Emergency Committee (EC) was convened on 19 May 2016. The WHO Director-General accepted the EC’s assessment that the urban yellow fever outbreaks in Angola and DRC are serious public health events which warrant intensified national action and enhanced international support. The situation does not currently constitute a Public Health Emergency of International Concern.
Vaccination
WHO Strategic Advisory Group of Experts (SAGE) on Immunization reviewed existing evidence that demonstrates that using a fifth of a standard vaccine dose would still provide protection against the disease for at least 12 months and possibly longer. This approach, known as fractional dosing, will be implemented in a pre-emptive mass vaccination campaign in DRC in Kinshasa.
Risk assessment
- The outbreak in Angola is receding and no confirmed case has been reported in the country during July (as of 21 July). The confirmed case with the most recent date of symptom onset, 23 June, was reported in Cuanhama district in Cunene province. However, a high level of vigilance needs to be maintained throughout the country.
- In DRC, the situation remains concerning as the outbreak has spread to three provinces. Given the presence and activity of the vector Aedes in the country, the outbreak might extend to other provinces, in particular Kasai, Kasai Central and Lualaba.
- Transmission of yellow fever in Angola and DRC is mainly concentrated in cities; however, there is a high risk of spread and local transmission to other provinces in both countries. In addition, the risk of potential spread to bordering countries, especially those classified as low-risk (i.e. Namibia, Zambia) and where the population, travelers and foreign workers are not vaccinated for yellow fever.
WHO: YF update from Africa
Sunday, July 10th, 2016Angola: 3552 suspected cases
In Angola, as of 1 July 2016 a total of 3552 suspected cases have been reported, of which 875 are confirmed. The total number of reported deaths is 355, of which 117 were reported among confirmed cases. Suspected cases have been reported in all 18 provinces and confirmed cases have been reported in 16 of 18 provinces and 80 of 125 reporting districts.
Mass vaccination campaigns first began in Luanda and have now expanded to cover most of the other affected parts of Angola. Recently, the campaigns have focused on border areas. Despite extensive vaccination efforts circulation of the virus persists.
Eleven reactive and pre-emptive mass vaccination campaigns are ongoing in several districts in Benguela, Huambo, Huila, Kwanza Norte, Kwanza Sul, Lunda Norte and Uige provinces. Six other mass vaccination campaigns are nearing completion. Mop-up campaigns are being implemented in parts of the provinces of Cunene, Lunda Norte, Uige and Zaire.
Democratic Republic of the Congo: 1307 suspected cases
There are no updates regarding the epidemiological situation in the Democratic Republic of The Congo (DRC). According to the latest available information (as of 24 June), the total number of notified suspected cases is 1307, with 68 confirmed cases and 75 reported deaths. Cases have been reported in 22 health zones in five of 26 provinces. Of the 68 confirmed cases, 59 were imported from Angola, two are sylvatic (not related to the outbreak) and seven are autochthonous.
In DRC, surveillance efforts have increased and vaccination campaigns have centred on affected health zones in Kinshasa and Kongo Central.
The risk of spread
Two additional countries have reported confirmed yellow fever cases imported from Angola: Kenya (two cases) and People’s Republic of China (11 cases). These cases highlight the risk of international spread through non-immunised travellers.
Seven countries (Brazil, Chad, Colombia, Ghana, Guinea, Peru and Uganda) are currently reporting yellow fever outbreaks or sporadic cases not linked to the Angolan outbreak.
Vaccination
WHO Strategic Advisory Group of Experts (SAGE) on Immunization reviewed existing evidence that demonstrates that using a fifth of a standard vaccine dose would still provide protection against the disease for at least 12 months and possibly longer. This approach, known as fractional dosing, is under consideration as a short-term measure, in the context of a potential vaccine shortage in emergencies.
Risk assessment
The outbreak in Angola remains of high concern due to:
- Persistent local transmission despite the fact that approximately 15 million people have been vaccinated;
- Local transmission has been reported in 12 highly populated provinces including Luanda.
- The continued extension of the outbreak to new provinces and new districts.
- High risk of spread to neighbouring countries. As the borders are porous with substantial cross-border social and economic activities, further transmission cannot be excluded. Viraemic travelling patients pose a risk for the establishment of local transmission especially in countries where adequate vectors and susceptible human populations are present;
- Risk of establishment of local transmission in other provinces where no autochthonous cases are reported;
- High index of suspicion of ongoing transmission in hard-to-reach areas like Cabinda;
In DRC, the outbreak has spread to three provinces. Given the limited availability of vaccines, the large Angolan community in Kinshasa, the porous border between Angola and DRC, and the presence and the activity of the vector Aedes in the country, the outbreak might extend to other provinces, in particular Kasai, Kasai Central and Lualaba.
The virus in Angola and DRC is largely concentrated in main cities; however, there is a high risk of spread and local transmission to other provinces in both countries. In addition, the risk is high for potential spread to bordering countries, especially those classified as low-risk (i.e. Namibia, Zambia) and where the population, travelers and foreign workers are not vaccinated for yellow fever.
Some African countries (Chad, Ghana, Guinea, Republic of Congo and Uganda) and some countries in South America (Brazil, Colombia and Peru) have reported cases of yellow fever in 2016. These events are not related to the Angolan outbreak, but there remains a need for vaccines in those countries, which poses additional strain on the limited global yellow fever vaccine stockpile.