Sunscreen: How to Help Protect Your Skin from the Sun
February 22nd, 2019What’s New
FDA regulates sunscreens to ensure they meet safety and effectiveness standards. To improve the quality, safety, and effectiveness of sunscreens, FDA issued a proposed rule on February 21, 2019 that describes updated proposed requirements for sunscreens. Given the recognized public health benefits of sunscreen use, Americans should continue to use sunscreen with other sun protective measures as this important rulemaking effort moves forward.
Additional information
Press Release
Infographic
Industry Fact Sheet
Consumer Update
Proposed rule
As an FDA-regulated product, sunscreens must pass certain tests before they are sold. But how you use this product, and what other protective measures you take, make a difference in how well you are able to protect yourself and your family from sunburn, skin cancer, early skin aging and other risks of overexposure to the sun. Some key sun safety tips include:
- Limit time in the sun, especially between the hours of 10 a.m. and 2 p.m., when the sun’s rays are most intense.
- Wear clothing to cover skin exposed to the sun, such as long-sleeved shirts, pants, sunglasses, and broad-brimmed hats.
- Use broad spectrum sunscreens with SPF values of 15 or higher regularly and as directed.
- Reapply sunscreen at least every two hours, and more often if you’re sweating or jumping in and out of the water.
Contents
Learn more about:
Read: Tips to Stay Safe in the Sun: From Sunscreen to Sunglasses
Watch: Videos about sunscreen
Learn: FDA Basics: Practice the art of sun protection
How to apply and store sunscreen
- Apply 15 minutes before you go outside. This allows the sunscreen (of SPF 15 or higher) to have enough time to provide the maximum benefit.
- Use enough to cover your entire face and body (avoiding the eyes and mouth). An average-sized adult or child needs at least one ounce of sunscreen (about the amount it takes to fill a shot glass) to evenly cover the body from head to toe.

Frequently forgotten spots:
Ears
Nose
Lips
Back of neck
Hands
Tops of feet
Along the hairline
Areas of the head exposed by balding or thinning hair
- Know your skin. Fair-skinned people are likely to absorb more solar energy than dark-skinned people under the same conditions.
- Reapply at least every two hours, and more often if you’re swimming or sweating.
There’s no such thing as waterproof sunscreen
People should also be aware that no sunscreens are “waterproof.” All sunscreens eventually wash off. Sunscreens labeled “water resistant” are required to be tested according to the required SPF test procedure. The labels are required to state whether the sunscreen remains effective for 40 minutes or 80 minutes when swimming or sweating, and all sunscreens must provide directions on when to reapply.
Storing your sunscreen
To keep your sunscreen in good condition, the FDA recommends that sunscreen containers should not be exposed to direct sun. Protect the sunscreen by wrapping the containers in towels or keeping them in the shade. Sunscreen containers can also be kept in coolers while outside in the heat for long periods of time. This is why all sunscreen labels must say: “Protect the product in this container from excessive heat and direct sun.”
Read: Tips to Stay Safe in the Sun: From Sunscreen to Sunglasses
Watch: Videos about sunscreen
Sunscreens for infants and children
Sunscreens are not recommended for infants. The FDA recommends that infants be kept out of the sun during the hours of 10 a.m. and 2 p.m., and to use protective clothing if they have to be in the sun. Infants are at greater risk than adults of sunscreen side effects, such as a rash. The best protection for infants is to keep them out of the sun entirely. Ask a doctor before applying sunscreen to children under six months of age.
For children over the age of six months, the FDA recommends using sunscreen as directed on the Drug Facts label.
Read: Should You Put Sunscreen on Infants? Not Usually.
Types of sunscreen
Sunscreen comes in many forms, including:
Lotions
Creams
Sticks
Gels
Oils
Butters
Pastes
Sprays
The directions for using sunscreen products can vary according to their forms. For example, spray sunscreens should never be applied directly to your face. This is just one reason why you should always read the label before using a sunscreen product.
Note: FDA has not authorized the marketing of nonprescription sunscreen products in the form of wipes, towelettes, powders, body washes, or shampoos.
Read: Use Sunscreen Spray? Avoid Open Flame.
Understanding the sunscreen label
Broad spectrum
Not all sunscreens are broad spectrum, so it is important to look for it on the label. Broad spectrum sunscreen provides protection from the sun’s ultraviolet (UV) radiation. There are two types of UV radiation that you need to protect yourself from – UVA and UVB. Broad spectrum provides protection against both by providing a chemical barrier that absorbs or reflects UV radiation before it can damage the skin.
Sunscreens that are not broad spectrum or that lack an SPF of at least 15 must carry the warning:
Sun protection factor (SPF)
Sunscreens are made in a wide range of SPFs.
The SPF value indicates the level of sunburn protection provided by the sunscreen product. All sunscreens are tested to measure the amount of UV radiation exposure it takes to cause sunburn when using a sunscreen compared to how much UV exposure it takes to cause a sunburn when not using a sunscreen. The product is then labeled with the appropriate SPF value. Higher SPF values (up to 50) provide greater sunburn protection. Because SPF values are determined from a test that measures protection against sunburn caused by UVB radiation, SPF values only indicate a sunscreen’s UVB protection.
As of June 2011, sunscreens that pass the broad spectrum test can demonstrate that they also provide UVA protection. Therefore, under the label requirements, for sunscreens labeled “Broad Spectrum SPF [value]”, they will indicate protection from both UVA and UVB radiation.
To get the most protection out of sunscreen, choose one with an SPF of at least 15.
If your skin is fair, you may want a higher SPF of 30 to 50.
There is a popular misconception that SPF relates to time of solar exposure. For example, many people believe that, if they normally get sunburned in one hour, then an SPF 15 sunscreen allows them to stay in the sun for 15 hours (e.g., 15 times longer) without getting sunburn. This is not true because SPF is not directly related to time of solar exposure but to amount of solar exposure.
The sun is stronger in the middle of the day compared to early morning and early evening hours. That means your risk of sunburn is higher at mid-day. Solar intensity is also related to geographic location, with greater solar intensity occurring at lower latitudes.
Sunscreen ingredients
Every drug has active ingredients and inactive ingredients. In the case of sunscreen, active ingredients are the ones that are protecting your skin from the sun’s harmful UV rays. Inactive ingredients are all other ingredients that are not active ingredients, such as water or oil that may be used in formulating sunscreens. Below is a list of acceptable active ingredients in products that are labeled as sunscreen:
Aminobenzoic acid
Avobenzone
Cinoxate
Dioxybenzone
Homosalate
Meradimate
Octocrylene
Octinoxate
Octisalate
Oxybenzone
Padimate O
Ensulizole
Sulisobenzone
Titanium dioxide
Trolamine salicylate
Zinc oxide
Although the protective action of sunscreen products takes place on the surface of the skin, there is evidence that at least some sunscreen active ingredients may be absorbed through the skin and enter the body. This makes it important to perform studies to determine whether, and to what extent, use of sunscreen products as directed may result in unintended, chronic, systemic exposure to sunscreen active ingredients.
Sunscreen expiration dates
FDA regulations require all sunscreens and other nonprescription drugs to have an expiration date unless stability testing conducted by the manufacturer has shown that the product will remain stable for at least three years. That means, a sunscreen product that doesn’t have an expiration date should be considered expired three years after purchase.
To make sure that your sunscreen is providing the sun protection promised in its labeling, the FDA recommends that you do not use sunscreen products that have passed their expiration date (if there is one), or that have no expiration date and were not purchased within the last three years. Expired sunscreens should be discarded because there is no assurance that they remain safe and fully effective.
Read: Don’t Be Tempted to Use Expired Medicine
Read: How to dispose of the outdated drugs
Sunscreens from other countries
In Europe and in some other countries, sunscreens are regulated as cosmetics, not as drugs, and are subject to different marketing requirements. Any sunscreen sold in the United States is regulated as a drug because it makes a drug claim – to help prevent sunburn or to decrease the risks of skin cancer and early skin aging caused by the sun.
If you purchase a sunscreen outside the United States, it is important to read the label to understand the instructions for use and any potential differences between the product and U.S. products.
Read: From our perspective: Helping to ensure the safety and effectiveness of sunscreens
Learn: FDA’s sunscreen guidance outlines safety and effectiveness data recommended for additional active ingredients
Additional Consumer Information
- Don’t Fry Day (the Friday before Memorial Day)
Protect your skin while enjoying the outdoors - CDC Sun Safety
- Skin Cancer Screening
- TanningThis site is intended to provide a source of general information on skin tanning, ultraviolet (UV) exposure, UV emitting products, and skin protection.
Regulatory Information
- Sunscreen Innovation Act
- Rulemaking History for monograph sunscreensRulemaking History for OTC Sunscreen Drug Products
- Questions and answers from 2011 labelling changes
At least 70 people have been killed and 40 injured after a fire tore through apartment buildings and chemical warehouses in a historic part of the Bangladesh capital Dhaka.
February 21st, 2019Two damning reports on the negative impact of climate change on global health……
February 21st, 2019“…..another dire warning about climate change, released yesterday in The Lancet, the New York Times reported. The report comes on the heels of the US government’s National Climate Assessment, which dropped on Black Friday—and echoes many of its findings. The 2 reports offer the gravest warning yet about the myriad, interconnected health risks of climate change….”
Quinta paciente contaminada pela bactéria Clostridium botulinum, causadora da doença de ‘Botulismo’.
February 21st, 2019
Significant Winter Storm to Continue Widespread Hazardous Weather Across the East
February 20th, 2019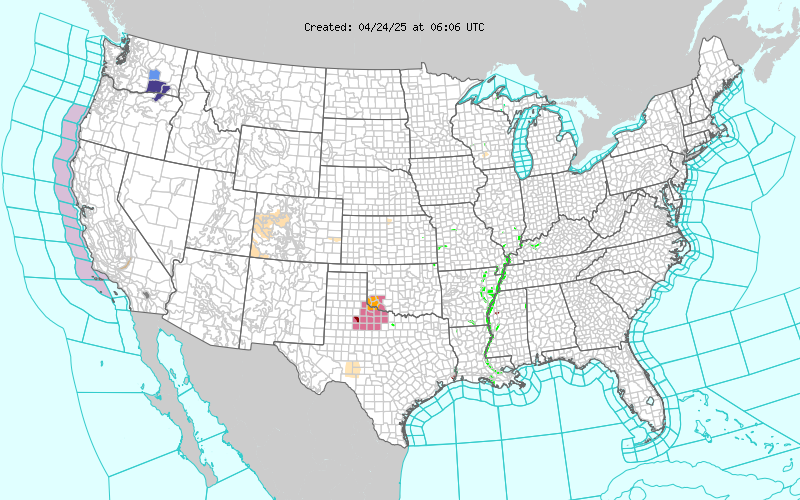

2/20/2003, West Warwick, Rhode Island: A fire at a rock concert in a nightclub kills 100 and seriously injures almost 200.
February 20th, 2019WHO: The health of displaced people in Europe
February 20th, 2019Copenhagen, Geneva, 21 January 2019
Migrants and refugees are likely to have good general health, but they can be at risk of falling sick in transition or while staying in receiving countries due to poor living conditions or adjustments in their lifestyle. This is the main conclusion of the first “Report on the health of refugees and migrants in the WHO European Region”, released by the WHO Regional Office for Europe today.
“Today, political and social systems are struggling to rise to the challenge of responding to displacement and migration in a humane and positive way. This report is the first of its kind, and gives us a snapshot of the health of refugees and migrants in the WHO European Region, at a time when the migration phenomenon is expanding across the world,” says Dr Zsuzsanna Jakab, WHO Regional Director for Europe.
The report summarizes the latest available evidence on the health of refugees and migrants in the WHO European Region – from a review of more than 13 000 documents – and the progress countries have made to promote their health. It was developed in partnership with the Italian National Institute for Health, Migration and Poverty (INMP).
Vulnerability to noncommunicable and communicable diseases
Refugees and migrants appear to be less affected than their host populations by many noncommunicable diseases on arrival; however, if they are in conditions of poverty, the duration of their stay in host countries increases their risk for cardiovascular diseases, stroke or cancer. As migrants and refugees are likely to change their lifestyle to engage in less physical activity and consume less healthy food, they are also more prone to risk factors for chronic diseases.
The displacement processes itself can make refugees and migrants more vulnerable to infectious diseases. Yet the report underlines that, for instance, the proportion of refugees and migrants among a host country’s tuberculosis (TB) cases varies broadly depending on the TB prevalence in the host population; and that a significant proportion of migrants and refugees who are HIV positive acquired the infection after they arrived in Europe. Despite the widespread assumption to the contrary, there is only a very low risk of refugees and migrants transmitting communicable diseases to their host population.
“The new report provides insight into what must be done to meet the health needs of both migrants and refugees and the host population. As migrants and refugees become more vulnerable than the host population to the risk of developing both noncommunicable and communicable diseases, it is necessary that they receive timely access to quality health services, as everyone else. This is the best way to save lives and cut treatment costs, as well as protect the health of the resident citizens,” stresses Dr Jakab.
Key findings and myths exposed
- International migrants make up only 10% (90.7 million) of the total population in the WHO European Region. Less than 7.4% of these are refugees. In some European countries, citizens estimate that there are 3 or 4 times more migrants than there really are.
- While communicable diseases are commonly linked with displacement and migration, there is a growing awareness that a range of acute and chronic conditions also require attention.
- Refugees and migrants are at lower risk for all forms of cancer, except cervical cancer. However, cancer in refugees and migrants is more likely to be diagnosed at an advanced stage, which can lead to considerably worse health outcomes than those of the host population.
- Depression and anxiety tend to affect refugees and migrants more than host populations. However, variation by migrant group and in the methods used to assess prevalence make it hard to draw firm conclusions.
- In general, refugees and migrants have a higher incidence, prevalence and mortality rate for diabetes than the host population, with higher rates in women.
- Refugees and migrants are potentially at greater risk of developing infectious diseases because of their exposure to infections, lack of access to health care, interrupted care and poor living conditions during the migration process. It is therefore necessary to protect them and to ensure that health-care workers on the front line understand the risks.
- While refugees and migrants may arrive in Europe with incomplete or interrupted immunization, vaccination uptake is likely to increase with the duration of their stay. The immediate response to new arrivals is to ensure that they receive basic vaccines based on the schedule of the host country.
- *Access to social and health services varies across the WHO European Region, with legal status, language barriers and discrimination generally being influential factors.
- *Unaccompanied minors are vulnerable to sexual exploitation and experience higher rates of depression and symptoms of post-traumatic stress disorder.
- *Male migrants experience significantly more work-related injuries than non-migrant workers.
A series of guidance documents was also developed to translate the report’s findings into practice. Each addresses a specific aspect of the health of refugees and migrants by providing tools, case studies and evidence to inform practices and policies to improve health. They focus on the areas of maternal and newborn health, children’s health, health promotion, mental health and healthy ageing. The documents were produced with financial support from the European Commission.
Towards refugee- and migrant-friendly health systems
Countries in the WHO European Region are making progress in implementing the Strategy and action plan for refugee and migrant health, adopted in 2016 by the WHO Regional Committee for Europe to guide progress on the health aspects of population movement. However, more needs to be done to progress towards refugee- and migrant-friendly health systems, including:
- providing quality and affordable health coverage as well as social protection for all refugees and migrants regardless of their legal status;
- making health systems culturally and linguistically sensitive to address communication barriers;
- ensuring health-care workers are well equipped and experienced to diagnose and manage common infectious and noninfectious diseases;
- enhancing multisectoral action on refugee and migrant health; and
- improving systematic and routine collection of comparable data on refugee and migrant health.
The WHO Regional Office for Europe and partners will continue to support the implementation of the Strategy and action plan, and to assist countries in filling potential gaps in health service delivery. This includes training health-care staff, providing technical assistance, carrying out joint public health and health system assessment missions, and providing policy recommendations using the WHO toolkit to prepare for large influxes of refugees and migrants.
Was it an “honor killing?”
February 19th, 2019“A court in Pakistan has acquitted the father, brother and uncle of a woman who died in a suspected honor killing last year.
Sana Cheema, 26, lived in Italy but died while visiting her family in Gujrat in April 2018.
She was originally buried without an autopsy – but when exhumed a cause of death was identified as strangulation…..”