The Saudi MOH has now confirmed 65 MERS infections since Jan 1
February 19th, 201918/02/2019 19-1841
MERS in Wadi Aldwasir city: 53-year-old male in Wadi Aldwasir city, Riyadh region
Contact with camels: Yes
Case classification: Primary
Current status: Hospitalized
This season’s flu vaccine efficacy: “….the overall estimated effectiveness of seasonal influenza vaccine for preventing medically attended, laboratory-confirmed influenza virus infection was 47%…”
February 18th, 2019“…..On the basis of data from the U.S. Influenza Vaccine Effectiveness Network on 3,254 children and adults with acute respiratory illness during November 23, 2018–February 2, 2019, the overall estimated effectiveness of seasonal influenza vaccine for preventing medically attended, laboratory-confirmed influenza virus infection was 47%.….”
Doyle JD, Chung JR, Kim SS, et al. Interim Estimates of 2018–19 Seasonal Influenza Vaccine Effectiveness — United States, February 2019. MMWR Morb Mortal Wkly Rep 2019;68:135–139. DOI: http://dx.doi.org/10.15585/mmwr.mm6806a2.
Flu Activity in the U.S. up to February 2, 2019: Maybe it isn’t as bad as we are led to believe!
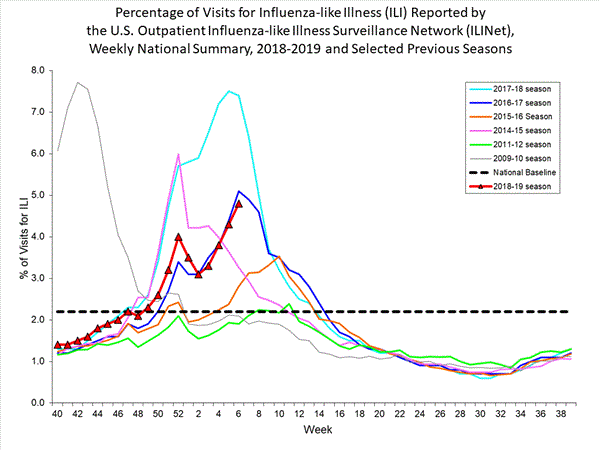
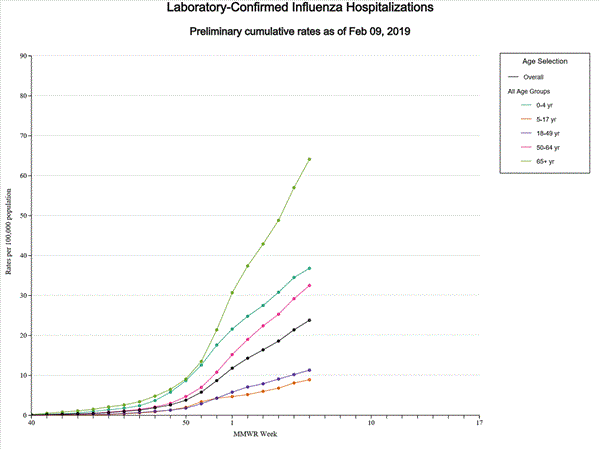
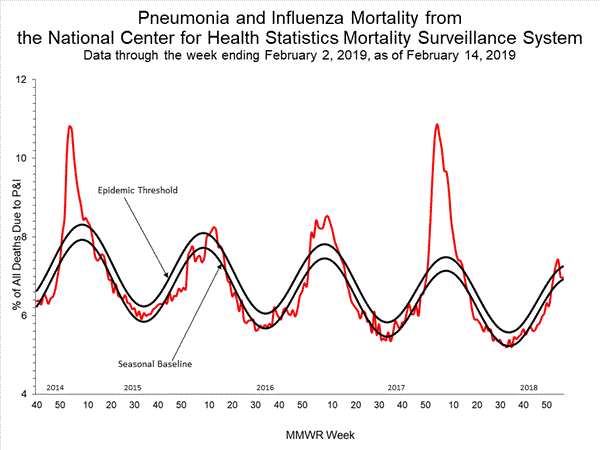
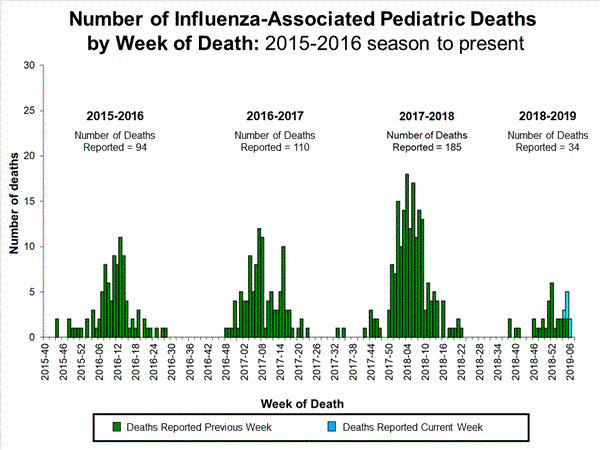
February 18th, 2019“……Influenza activity in the United States remained elevated through February 2, 2019, and is expected to continue for several more weeks. Compared with recent influenza seasons, as of February 2, 2019, severity this season has been low, with a lower percentage of outpatient visits for influenza-like illness, lower rates of hospitalization, and fewer deaths attributed to pneumonia and influenza…..”
Blanton L, Dugan VG, Abd Elal AI, et al. Update: Influenza Activity — United States, September 30, 2018–February 2, 2019. MMWR Morb Mortal Wkly Rep 2019;68:125–134. DOI: http://dx.doi.org/10.15585/mmwr.mm6806a1.
Guatemala, 2017: After hours of incarceration someone lit a match. Fire, a locked door, guards nearby, and 41 girls dies
February 18th, 2019Another MERS case in Saudi Arabia, making it 62 for the year
February 18th, 2019Middle East respiratory syndrome coronavirus (MERS-CoV) – Saudi Arabia
From 1 January through 31 January 2019, the International Health Regulations (IHR) National Focal Point of Saudi Arabia reported fourteen additional cases of Middle East respiratory syndrome coronavirus (MERS-CoV) infection, including three deaths. Details of these cases can be found by following the link to a separate document after this paragraph. Of the 14 cases reported in January, eight are from three separate clusters of cases. Cluster 1 involves three cases (listed as cases 1, 2 and 3) in Riyadh Province and cluster 2 involves two cases (listed as cases 4 and 5) in the city of Jeddah. Cluster 3 involves three cases (listed as cases 11, 13 and 14) in the city of Wadi Aldwaser and is currently ongoing. More details regarding the outbreak in Wadi Aldwaser and the implementation of interventions by the Ministry of Health (MoH) in Saudi Arabia will be provided in the next update.

The link below provides details of the fourteen reported additional cases.
From 2012 through 31 January 2019, the total number of laboratory-confirmed MERS-CoV cases reported globally to WHO under IHR (2005) is 2 298 with 811 associated deaths. The total number of deaths includes the deaths that WHO is aware of to date through follow-up with affected member states.
WHO risk assessment
Infection with MERS-CoV can cause severe disease resulting in high mortality. Humans are infected with MERS-CoV from direct or indirect contact with dromedary camels. MERS-CoV has demonstrated the ability to transmit between humans. So far, the observed non-sustained human-to-human transmission has occurred mainly in health care settings.
As of 15 February 2019, there is an ongoing outbreak of MERS in Wadi Aldwaser, which includes cases 11, 13 and 14 reported in the separate document linked above. WHO will provide details of the additional cases involved in this outbreak as well as intervention measures implemented by the MoH. The notification of additional cases does not change the overall risk assessment. WHO expects that additional cases of MERS-CoV infection will be reported from the Middle East, and that cases will continue to be exported to other countries by individuals who might acquire the infection after exposure to dromedary camels, animal products (for example, consumption of camel’s raw milk), or humans (for example, in a health care setting). WHO continues to monitor the epidemiological situation and conducts risk assessment based on the latest available information.
WHO advice
Based on the current situation and available information, WHO encourages all Member States to continue their surveillance for acute respiratory infections and to carefully review any unusual patterns.
Infection prevention and control measures are critical to prevent the possible spread of MERS-CoV in health care facilities. It is not always possible to identify patients with MERS-CoV early because like other respiratory infections, the early symptoms of MERS-CoV are non-specific. Therefore, healthcare workers should always apply standard precautions consistently with all patients, regardless of their diagnosis. Droplet precautions should be added to the standard precautions when providing care to patients with symptoms of acute respiratory infection; contact precautions and eye protection should be added when caring for probable or confirmed cases of MERS-CoV infection; airborne precautions should be applied when performing aerosol generating procedures. Early identification, case management and isolation, together with appropriate infection prevention and control measures can prevent human-to-human transmission of MERS-CoV.
MERS-CoV appears to cause more severe disease in people with diabetes, renal failure, chronic lung disease, and immunocompromised persons. Therefore, these people should avoid close contact with animals, particularly dromedary camels, when visiting farms, markets, or barn areas where the virus is known to be potentially circulating. General hygiene measures, such as regular hand washing before and after touching animals and avoiding contact with sick animals, should be adhered to. Food hygiene practices should be observed. People should avoid drinking raw camel milk or camel urine, or eating meat that has not been properly cooked.
WHO does not advise special screening at points of entry with regard to this event nor does it currently recommend the application of any travel or trade restrictions.
From 1 January through 10 February 2019, 327 cases of Lassa fever (324 confirmed cases and three probable cases) with 72 deaths (case fatality ratio = 22%) have been reported in Nigeria
February 17th, 2019Lassa Fever – Nigeria
From 1 January through 10 February 2019, 327 cases of Lassa fever (324 confirmed cases and three probable cases) with 72 deaths (case fatality ratio = 22%) have been reported across 20 states and the Federal Capital Territory, with the majority of cases being reported from Edo (108) and Ondo (103) states. Twelve cases have been reported among healthcare workers in seven states – Edo (4), Ondo (3), Ebonyi (1), Enugu (1), Rivers (1), Bauchi (1) and Benue (1) including one death in Enugu.
The number of confirmed cases reported across Nigeria remains high. In week 6, 2019 (week ending 10 February 2019), 37 new confirmed cases including 10 deaths (case fatality ratio = 27%) were reported from nine states across Nigeria. The majority of cases were reported from Ondo (12) and Edo (10) states. The number of confirmed cases reported in week 6, 2019 represents a slight decrease compared to week 5 when 68 confirmed cases were reported (Figure 1).
Of the 3746 contacts identified since January 2019, 2658 are still under follow-up while 1045 have completed 21 days of follow-up. Sixty contacts became symptomatic, of which 39 tested positive.
Ninety-one case-patients are currently in admission at treatment centers across the country. The case-patients are being treated with standard supportive care.
Figure 1: Number of confirmed and probable Lassa fever cases in Nigeria reported by the week of illness onset from 1 January through 10 February 2019
Source: Nigeria Centre for Disease Control (NCDC)
Public health response
- On 22 January 2019, the Nigeria Center for Disease Control (NCDC) declared the outbreak an emergency.
- Multi-sectoral One Health national rapid response teams have been deployed to Ondo, Edo, Ebonyi, Plateau, and Bauchi to support field investigation and response activities.
- Enhanced surveillance is ongoing in all states following alert communication and a press release from NCDC.
- Treatment of Lassa fever cases is also ongoing at designated treatment centres across the country.
- Risk communication and community engagement activities continue in the states. National awareness was improved through the recently concluded international Lassa fever conference which took place from 16 through 17 January 2019.
WHO risk assessment
Lassa fever is a viral haemorrhagic fever that is transmitted to humans via contact with food or household items contaminated with rodent urine or faeces. Person-to-person infections and laboratory transmission can also occur. The overall case fatality rate is 1%; it is 15% among patients hospitalized with severe illness. There is currently no approved vaccine. Early supportive care with rehydration and symptomatic treatment improves survival.
Although Lassa fever is known to be endemic in Nigeria with the peak season anticipated from December through June, the current increase in new confirmed cases and deaths should be monitored closely and addressed appropriately. Cases in neigbouring Benin and Togo potentially originating from Nigeria have been reported in previous years and therefore neighbouring countries should be monitored accordingly.
With twelve confirmed cases so far among healthcare workers, there is evidence of nosocomial transmission of the disease amidst reports of inadequate infection prevention and control (IPC) supplied in some health facilities and complacency on the part of health workers towards maintaining IPC measures.
WHO advice
Prevention of Lassa fever relies on community engagement and promoting hygienic conditions to discourage rodents from entering homes. In healthcare settings, staff should consistently implement standard infection prevention and control measures when caring for patients to prevent nosocomial infections. WHO continues to advice all countries in the Lassa fever belt on the need to enhance early detection and treatment of cases to reduce the case fatality rate as well as strengthen cross-border collaboration.
WHO does not recommend any travel or trade restriction to Nigeria based on the currently available information.
For more information on Lassa fever, please see the link below:
Venezuela is in worse shape than Syria?
February 17th, 2019“…..In 2017, more than 280,000 children were found to be malnourished and at risk of dying. The situation in the country has only declined drastically and the statistics are likely far worse now. Alarmingly, the government denies there are any problems; it doesn’t even allow health statistics to be officially kept.
Still, we know that newborns in Syria, which is still wracked by war, are more likely to survive than those born to Venezuelan mothers; maternal mortality rose 66 percent from 2015 to 2016. The average person in the nation lost 24 pounds in 2017.Reports indicate that nearly 80 percent of hospitals lack regular access to water, 53 percent of the nation’s operating rooms are shuttered and more than 70 percent of emergency rooms cannot regularly provide services to patients….”
2018-2019 Influenza Season Week 6 ending February 9, 2019: Influenza activity continues to increase in the United States.
February 16th, 2019DRC: Ebola cases climb to 835
February 16th, 2019Ebola virus disease – Democratic Republic of the Congo
Despite slightly fewer cases reported during the past week (Figure 1), current epidemiological indicators highlight that the Ebola virus disease (EVD) outbreak is continuing with moderate intensity. Katwa and Butembo remain the major health zones of concern, while simultaneously, small clusters continue to occur in various geographically dispersed regions. During the last 21 days (23 January – 12 February 2019), 97 new cases have been reported from 13 health zones (Figure 2), including: Katwa (59), Butembo (12), Beni (7), Kyondo (4), Oicha (4), Vuhovi (3), Biena (2), Kalunguta (2), Komanda (1), Manguredjipa (1), Mabalako (1), Masereka (1), and Mutwanga (1).1 The recent case reported in the Komanda health zone was a resident of Katwa who was exposed to the virus, and subsequently travelled to both Bunia and Komanda. This case comes one month after the last reported case in Ituri Province; underscoring the high risks of reintroduction to previously affected areas, as well as the potential for spread to new ones.
As of 12 February, 823 EVD cases2 (762 confirmed and 61 probable) have been reported, including 517 deaths (overall case fatality ratio: 63%). Cumulatively, cases have been reported from 118 of 287 health areas across 18 health zones, of which 37 health areas have reported a case in the last 21 days. Thus far, 283 people have been discharged from Ebola Treatment Centers (ETCs) and enrolled in a dedicated monitoring and support programme. One new health worker infection was reported in Katwa. To date, a total of 68 health workers have been infected.
Main challenges this past week primarily pertain to community mistrust, particularly in Katwa, and the difficulty in encouraging community members to be more proactive in reporting suspected cases, presenting early to ETCs for treatment, and participating in community-based prevention and response efforts. However, in the face of these protracted challenges, response strategies have demonstrated to be effective in curtailing the spread of EVD. Fostering greater community trust by strengthening engagement with its members remains a top priority for response teams.
On 13 February, the Ministry of Health (MoH) launched the Strategic Response Plan 3 (SRP 3). The plan lays out the response strategy, objectives and budget requirements for the MoH, WHO, and all implementing partners for the next six months (February through July 2019). SRP 3 takes into account recommendations from operational reviews, and builds on a series of new strategic directions that capitalize on lessons learned under the scope of SRP 2. Activities laid out aim to stop the transmission of EVD in North Kivu and Ituri provinces, and prevent its spread to other provinces and neighbouring countries.
WHO remains confident that this outbreak can be successfully brought to an end through strategies outlined in SRP 3. To achieve the goals set out by the plan, MoH, WHO, and partners are appealing for US$ 148 million. WHO and partners count on the continued support of the international community to provide the required funding in order to stop this outbreak.
Figure 1: Confirmed and probable Ebola virus disease cases by week of illness onset, data as of 12 February 2019 (n=822)
Figure 2: Confirmed and probable Ebola virus disease cases reported between 22 January and 11 February by place of residence, North Kivu and Ituri provinces, Democratic Republic of the Congo (n=101)*
*Map based on the latest available detailed line lists (data as of 11 February 2019), and excludes cases reported after this date, as well as cases with delayed/missing village or health area details. Categorization of cases by health zone may differ from the reported place of residence.
Public health response
For further information about the public health response actions by the MoH, WHO, and partners, please refer to the latest situation reports published by the WHO Regional Office for Africa:
WHO risk assessment
WHO continuously monitors changes to the epidemiological situation and context of the outbreak to ensure that support to the response is adapted to the evolving circumstances. The last review conducted on 7 February 2019, outlines the high risk the EVD outbreak poses at the national and regional levels, though global risk levels remain low. This EVD outbreak is affecting primarily the north-eastern provinces of the Democratic Republic of the Congo bordering Uganda, Rwanda, and South Sudan. There is a potential risk for transmission of EVD at the national and regional levels due to extensive travel between the affected areas, the rest of the country, and neighbouring countries for economic and personal reasons, as well as due to insecurity. The country is concurrently experiencing other epidemics (e.g. cholera, vaccine-derived poliomyelitis, malaria), and a long-term humanitarian crisis. Additionally, the fragile security situation in North Kivu and Ituri, further limits the implementation of response activities.
As the risk of national and regional spread is very high, it is important for neighbouring provinces and countries to enhance surveillance and preparedness activities. The International Health Regulations (IHR 2005) Emergency Committee has advised that failing to intensify these preparedness and surveillance activities would lead to worsening conditions and further spread. WHO will continue to work with neighbouring countries and partners to ensure that health authorities are alerted and are operationally prepared to respond.
WHO advice
International traffic: WHO advises against any restriction of travel to, and trade with, the Democratic Republic of the Congo based on the currently available information. There is currently no licensed vaccine to protect people from the Ebola virus. Therefore, any requirements for certificates of Ebola vaccination are not a reasonable basis for restricting movement across borders or the issuance of visas for passengers leaving the Democratic Republic of the Congo. WHO continues to closely monitor and, if necessary, verify travel and trade measures in relation to this event. Currently, no country has implemented travel measures that significantly interfere with international traffic to and from the Democratic Republic of the Congo. Travellers should seek medical advice before travel and should practice good hygiene.
For more information, see:
- South Sudan vaccinates health workers against Ebola
- Ebola – Following a Full Simulation Exercise, a Joint Monitoring Mission is deployed in Rwanda
- Summary report for the SAGE meeting of October 2018
- Statement on the October 2018 meeting of the IHR Emergency Committee on the Ebola virus disease outbreak in the Democratic Republic of the Congo
- WHO Interim recommendation Ebola vaccines
- WHO recommendations for international travellers related to the Ebola Virus Disease outbreak in the Democratic Republic of the Congo
- Ebola virus disease in the Democratic Republic of the Congo – Operational readiness and preparedness in neighbouring countries
- Ebola virus disease fact sheet
1 Excludes newly probable cases from Katwa (7) and Komanda (5), who died in November and December 2018 and were reported during the period of 21 January to 10 February following a retrospective re-classification of cases.
2 Data in recent weeks are subject to delays in case confirmation and reporting, as well as ongoing data cleaning – trends during this period should be interpreted cautiously.