US: Measles Cases in 2019
February 13th, 2019Measles Cases in 2019
From January 1 to February 7, 2019, 101** individual cases of measles have been confirmed in 10 states.
The states that have reported cases to CDC are California, Colorado, Connecticut, Georgia, Illinois, New Jersey, New York, Oregon, Texas, and Washington.

*Cases as of December 29, 2018. Case count is preliminary and subject to change.
**Cases as of February 7, 2019. Case count is preliminary and subject to change. Data are updated weekly.
Measles Outbreaks in 2019
Five outbreaks (defined as 3 or more cases) have been reported in 2019 in the following jurisdictions:
These outbreaks are linked to travelers who brought measles back from other countries such as Israel and Ukraine, where large measles outbreaks are occurring. Make sure you are vaccinated against measles before traveling internationally.
Spread of Measles
- The majority of people who got measles were unvaccinated.
- Measles is still common in many parts of the world including some countries in Europe, Asia, the Pacific, and Africa.
- Travelers with measles continue to bring the disease into the U.S.
- Measles can spread when it reaches a community in the U.S. where groups of people are unvaccinated.
Measles Outbreaks
In a given year, more measles cases can occur for any of the following reasons:
- an increase in the number of travelers who get measles abroad and bring it into the U.S., and/or
- further spread of measles in U.S. communities with pockets of unvaccinated people.
Reasons for an increase in cases some years:
- 2018: The U.S. experienced 17 outbreaks in 2018, including three outbreaks in New York State, New York City, and New Jersey, respectively. Cases in those states occurred primarily among unvaccinated people in Orthodox Jewish communities. These outbreaks were associated with travelers who brought measles back from Israel, where a large outbreak is occurring. Eighty-two people brought measles to the U.S. from other countries in 2018. This is the greatest number of imported cases since measles was eliminated from the U.S. in 2000.
- 2017: A 75-case outbreak was reported in Minnesota in a Somali-American community with poor vaccination coverage.
- 2015: The United States experienced a large (147 cases), multi-state measles outbreak linked to an amusement park in California. The outbreak likely started from a traveler who became infected overseas with measles, then visited the amusement park while infectious; however, no source was identified. Analysis by CDC scientists showed that the measles virus type in this outbreak (B3) was identical to the virus type that caused the large measles outbreak in the Philippines in 2014.
- 2014: The U.S. experienced 23 measles outbreaks in 2014, including one large outbreak of 383 cases, occurring primarily among unvaccinated Amish communities in Ohio. Many of the cases in the U.S. in 2014 were associated with cases brought in from the Philippines, which experienced a large measles outbreak.
- 2013: The U.S. experienced 11 outbreaks in 2013, three of which had more than 20 cases, including an outbreak with 58 cases. For more information see Measles — United States, January 1-August 24, 2013.
- 2011: In 2011, more than 30 countries in the WHO European Region reported an increase in measles, and France was experiencing a large outbreak. These led to a large number of importations (80) that year. Most of the cases that were brought to the U.S. in 2011 came from France. For more information see Measles — United States, January-May 20, 2011.
- 2008: The increase in cases in 2008 was the result of spread in communities with groups of unvaccinated people. The U.S. experienced several outbreaks in 2008 including three large outbreaks. For more information see Update: Measles — United States, January–July 2008.
See also: The Surveillance Manual chapter on measles that describes case investigation, outbreak investigation, and outbreak control for additional information.
An enormous blaze broke out at a fully occupied hotel in central New Delhi on Tuesday morning, killing at least 17
February 12th, 2019MERS-CoV cases announced from Wadi al-Dawasir
February 12th, 201903/02/2019 19-1793
MERS in Riyadh city: 75-year-old male in Riyadh city, Riyadh region Contact with camels: No Case classification: Primary, community acquired Current status: Hospitalized
ﻣ ﺔﻣزﻼﺘ قﺮﺸﻟا ﻂﺳوﻷا ﺔﻴﺴﻔﻨﺘﻟا ﻦﻣ ﺔﻨﻳﺪﻣ اﻟﺮﻳﺎض: ﻣﻨﻄﻘﺔ اﻟﺮﻳﺎض ، ﻋﺎ ًﻣﺎ ﻦﻣ ﺔﻨﻳﺪﻣ اﻟﺮﻳﺎض 75 ﻞﺟر ﻳ ﻎﻠﺒ ﺔﻄﻟﺎﺨﻣ ﻞﺑﻺﻟ ﻻ: ﻣﻜﺘﺴﺒﺔ ﻓﻲ اﻟﻤﺠﺘﻤﻊ ، ﻒﻴﻨﺼﺗ ﺔﻟﺎﺤﻟا أ:ﺔﻴﻟو ﺔﻟﺎﺣ اﻟﻤﺮﻳﺾ :مﻮﻨﻣ ﻲﻓ اﻟﻤﺴﺘﺸﻔﻰ
03/02/2019 19-1794
MERS in Wadi Aldwasir city: 55-year-old male in Wadi Aldwasir city, Riyadh region Contact with camels: Yes Case classification: Secondary, healthcare-acquired Current status: Hospitalized
ﻣ ﺔﻣزﻼﺘ قﺮﺸﻟا ﻂﺳوﻷا ﺔﻴﺴﻔﻨﺘﻟا ﻦﻣ ﺔﻨﻳﺪﻣ يداو ، ﻋﺎ ًﻣﺎ ﻦﻣ ﺔﻨﻳﺪﻣ يداو اﻟﺪواﺳﺮ 55 اﻟﺪواﺳﺮ: ﻞﺟر ﻳ ﻎﻠﺒ ﺔﻘﻄﻨﻣ اﻟﺮﻳﺎض ﺔﻄﻟﺎﺨﻣ ﻞﺑﻺﻟ :ﻢﻌﻧ ﻣﻜﺘﺴﺒﺔ ﻓﻲ ﻣﻨﺸﺄة ﺔﻴﺤﺻ ، ﻒﻴﻨﺼﺗ ﺔﻟﺎﺤﻟا :ﺔﻳﻮﻧﺎﺛ ﺔﻟﺎﺣ اﻟﻤﺮﻳﺾ :مﻮﻨﻣ ﻲﻓ اﻟﻤﺴﺘﺸﻔﻰ
03/02/2019 19-1795
MERS in Wadi Aldwasir city: 40-year-old male in Wadi Aldwasir city, Riyadh region Contact with camels: yes Case classification: Secondary, household contact Current status: Hospitalized
Hooch in Uttar Pradesh: The death toll of the hooch tragedy climbed up to 92 on Saturday
February 12th, 2019“……So far, 39 people were arrested in Saharanpur while 35 cases have been registered in the area….. The police conducted raids on illegal liquor shops across the state……”
Latest research: “End-of-season influenza vaccine efficacy for the 2017-2018 flu season was a mediocre 38% (95% CI 31%-43%), but flu shots were still estimated to have prevented 7 million illnesses and 8,000 deaths…”
February 11th, 2019Effects of Influenza Vaccination in the United States during the 2017–2018 Influenza Season
HIV, circumcision & Tanzanian members of Parliament
February 11th, 2019“A female MP in Tanzania has called for checks to determine whether or not her male colleagues have undergone circumcision – a procedure known to reduce the risk of HIV transmission……The World Health Organization (WHO) says circumcision reduces the risk of heterosexual men contracting HIV by around 60%……”
DRC and EBV: Outbreak totals now stand at 800 cases, including 502 deaths, and 178 suspected cases are still under investigation.
February 11th, 2019SITUATION ÉPIDÉMIOLOGIQUE DANS LES PROVINCES DU NORD-KIVU ET DE L’ITURI
Vendredi 8 février 2019
- Depuis le début de l’épidémie, le cumul des cas est de 800, dont 739 confirmés et 61 probables. Au total, il y a eu 502 décès (441 confirmés et 61 probables) et 271 personnes guéries.
- 178 cas suspects en cours d’investigation.
- 2 nouveaux cas confirmés, dont 1 à Oicha et 1 à Kyondo
- 3 nouveaux décès de cas confirmés :
- 1 décès communautaire à Kyondo
- 2 décès au CTE, dont 1 à Butembo et 1 à Katwa
- 7 nouveaux cas probables (décès historiques) validés à Katwa.
- Plus d’informations à ce sujet seront fournis dans le bulletin du samedi 9 février 2019.
- 4 nouvelles personnes guéries sorties du CTE de Butembo.

2018-2019 Influenza Season Week 5 ending February 2, 2019: Influenza activity increased in the United States.
February 9th, 2019Influenza activity increased in the United States. Influenza A(H1N1)pdm09, influenza A(H3N2), and influenza B viruses continue to co-circulate. Below is a summary of the key influenza indicators for the week ending February 2, 2019
- Viral Surveillance:The percentage of respiratory specimens testing positive for influenza viruses in clinical laboratories increased. Influenza A viruses have predominated in the United States since the beginning of October. Influenza A(H1N1)pdm09 viruses have predominated in most areas of the country, however influenza A(H3) viruses have predominated in the southeastern United States (HHS Region 4).
- Virus Characterization:The majority of influenza viruses characterized antigenically and genetically are similar to the cell-grown reference viruses representing the 2018–2019 Northern Hemisphere influenza vaccine viruses.
- Antiviral Resistance:The vast majority of influenza viruses tested (>99%) show susceptibility to oseltamivir and peramivir. All influenza viruses tested showed susceptibility to zanamivir.
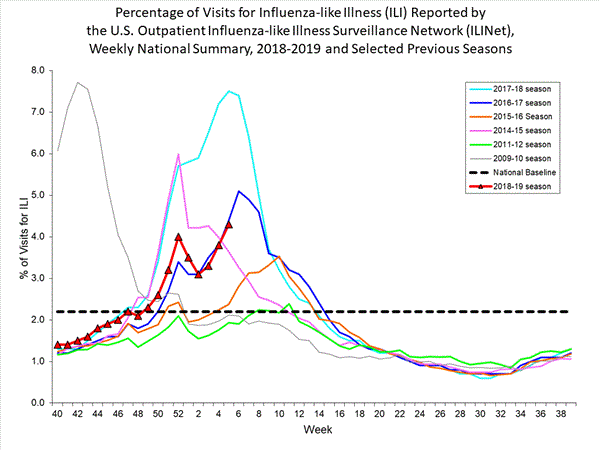
- Influenza-like Illness Surveillance:The proportion of outpatient visits for influenza-like illness (ILI) increased to 4.3%, which is above the national baseline of 2.2%. All 10 regions reported ILI at or above their region-specific baseline level.
- ILI State Activity Indictor Map: New York City and 24 states experienced high ILI activity; Puerto Rico and 10 states experienced moderate ILI activity; the District of Columbia and 13 states experienced low ILI activity; and three states experienced minimal ILI activity.
- Geographic Spread of Influenza: The geographic spread of influenza in Puerto Rico and 47 states was reported as widespread; two states reported regional activity; the District of Columbia and one state reported local activity; the U.S. Virgin Islands reported sporadic activity; and Guam did not report.
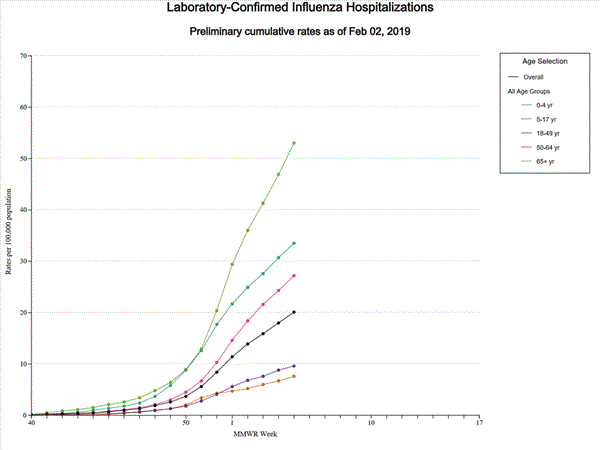
- Influenza-associated Hospitalizations A cumulative rate of 20.1 laboratory-confirmed influenza-associated hospitalizations per 100,000 population was reported. The highest hospitalization rate is among adults 65 years and older (53.0 hospitalizations per 100,000 population).
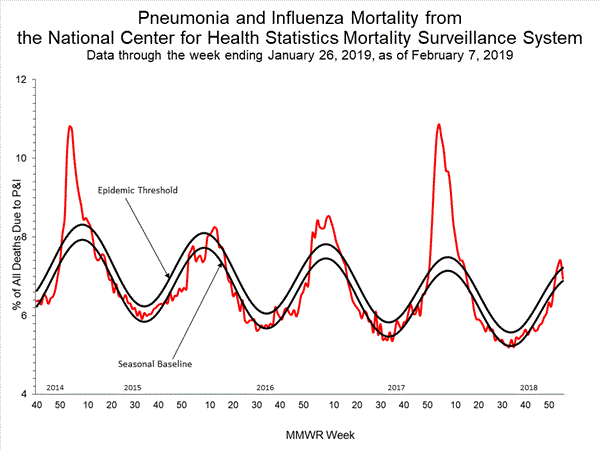
- Pneumonia and Influenza Mortality: The proportion of deaths attributed to pneumonia and influenza (P&I) was below the system-specific epidemic threshold in the National Center for Health Statistics (NCHS) Mortality Surveillance System.
- Influenza-associated Pediatric Deaths: Four influenza-associated pediatric deaths were reported to CDC during week 5.
An increase in reports of acute flaccid paralysis (AFP) in the United Kingdom, 1 January 2018–21 January 2019.
February 8th, 2019“…..As at 21 January 2019, 40 cases had been identified with a peak in October 2018. The increase was temporally associated with an upsurge in enterovirus (EV) D68 activity. Enterovirus was detected in 15 cases, mainly from respiratory tract samples; nine were typed as EV-D68……”
Measles Red Flag in the Philippines
February 8th, 2019he Department of Health (DOH) raised today the red flag for measles in other regions of Luzon, Central and Eastern Visayas aside from yesterday’s declaration in the National Capital Region.
As of 26 January 2019, validated data from CALABARZON was 575 cases with 9 deaths (CFR 2%) (2,538% an increase as compared to 21 cases of 2018), NCR was 441 with 5 deaths (CFR 1%) (1,125% increase as compared to 36 cases of 2018), Region 3 had 192 cases with 4 deaths (CFR 2%) (500% increase compared to 32 cases of 2018), Region 6 with 104 cases and 3 deaths (CFR 3%) (550% increase compared to 16 cases of 2018) and Region 7 with 71 cases with 1 death (CFR 1%) (3,450% increase compared to 2 cases of 2018).
“We are expanding the outbreak from Metro Manila to the other regions as cases have increased in the past weeks and to strengthen surveillance of new cases and alert mothers and caregivers to be more vigilant,” Health Secretary Francisco T. Duque III said.
Other regions showed the number of cases reported at 70 cases with no deaths for MIMAROPA (3,400% increase compared to 2 cases of 2018), Region 1 with 64 cases with 2 deaths (CFR 3%) (220% increase compared to 20 cases of 2018), Region 10 with 60 cases with no deaths reported (4% decrease compared to 63 cases in 2018), Region 8 with 54 cases and 1 death (2% CFR) (5,300% increase compared to 1 case of 2018), Region 12 with 43 cases with no deaths (34% decrease compared to 66 cases of 2018). These regions should likewise step-up their response against this highly communicable disease, as well as ensure that preventive measures play a vital role in preventing the spread of the disease; these must be emphasized to mothers and the general public as a whole.
Measles is a highly contagious respiratory disease caused by a virus. It is transferred from person-to-person by sneezing, coughing, and close personal contact. Its signs and symptoms include cough, runny nose, red eyes/conjunctivitis, fever, skin rashes lasting for more than 3 days.
The disease’s complications included diarrhea, middle ear infection, pneumonia (infection of the lungs), encephalitis (swelling of the brain), malnutrition, blindness which may lead to death.
“Supportive measures like building the nutritional status of the sick person and increasing oral rehydration are important measures to increase body resistance and replace lost body fluids caused by coughing, diarrhea, and perspiration,” Duque said, adding that immunization and vitamin A supplementation of nine-month old children and unvaccinated individuals are the best defenses against measles.
The DOH is advising mothers, the public to bring their children at the first sign of fever to the nearest health facility for prompt treatment and proper case management.