Archive for January, 2016
WHO: Globally, 41 million children under 5 years of age are obese or overweight.
Tuesday, January 26th, 2016An unusual increase of Guillain-Barré Syndrome (GBS) in El Salvador
Tuesday, January 26th, 2016Guillain-Barré syndrome – El Salvador
The National IHR Focal Point of El Salvador has notified PAHO/WHO of an unusual increase of Guillain-Barré Syndrome (GBS) in the country. In El Salvador, the annual average number of GBS is 169; however, from 1 December 2015 to 6 January 2016, 46 GBS were recorded, including 2 deaths.
Of the 46 GBS cases, 25 (54%) are male and 35 (76%) are 30 years old or older. All cases were hospitalized and treated with plasma exchange or intravenous immunoglobulin. One of the two deceased patients had a history of multiple underlying chronic diseases. Out of the 22 patients whose information was available, 12 (54%) presented with febrile rash illness in the 15 days prior to the onset of symptoms consistent with GBS.
Investigations are ongoing to determine the cause of infection and acquire further details about the laboratory diagnosis. Possible associations between GBS and Zika virus infection are also being investigated. Since the confirmation of the first case of Zika virus infection in November 2015 until 31 December 2015, Salvadoran health authorities reported 3,836 suspected cases of Zika virus infection.
CDC
“……What is Guillain-Barré syndrome (GBS)? Guillain-Barré syndrome (GBS) is a rare disorder in which a person’s own immune system damages their nerve cells, causing muscle weakness and sometimes paralysis. GBS can cause symptoms that usually last for a few weeks. Most people recover fully from GBS, but some people have long-term nerve damage. In very rare cases, people have died of GBS, usually from difficulty breathing. In the United States, for example, an estimated 3,000 to 6,000 people develop GBS each year on average……”
Grappling with Zika virus’ link to microcephaly, El Salvador is advising all women in the country not to get pregnant until 2018.
Tuesday, January 26th, 2016** WHO: The mosquito-borne Zika virus is expected to spread to all countries in the Americas except for Canada and Chile.
Monday, January 25th, 2016CDC: Schuler-Faccini L, Ribeiro EM, Feitosa IM, et al. Possible Association Between Zika Virus Infection and Microcephaly — Brazil, 2015. MMWR Morb Mortal Wkly Rep 2016;65(Early Release):1–4. DOI: http://dx.doi.org/10.15585/mmwr.mm6503e2er.
CDC: Hennessey M, Fischer M, Staples JE. Zika Virus Spreads to New Areas — Region of the Americas, May 2015–January 2016. MMWR Morb Mortal Wkly Rep 2016;65(Early Release):1–4. DOI: http://dx.doi.org/10.15585/mmwr.mm6503e1er.
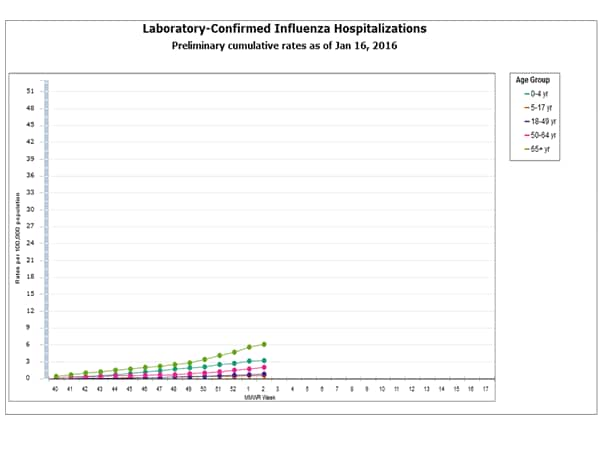
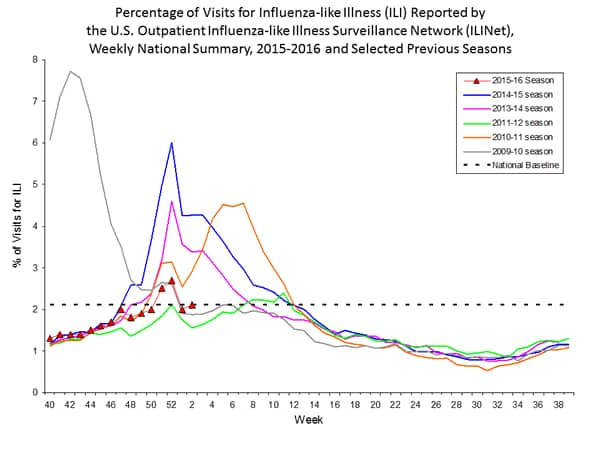
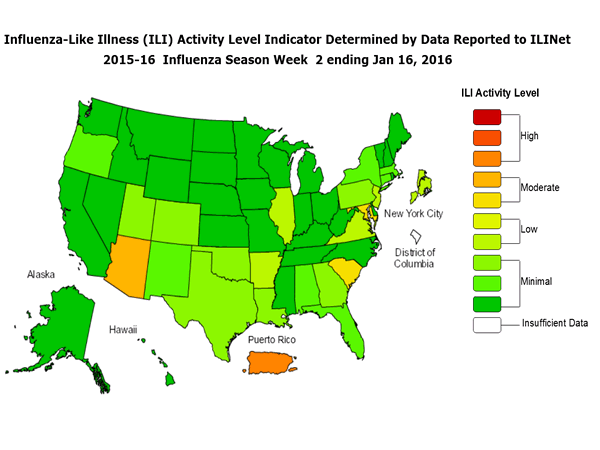
2015-2016 Influenza Season Week 2 ending January 16, 2016
Sunday, January 24th, 2016During week 2 (January 10-16, 2016), influenza activity increased slightly in the United States.
- Viral Surveillance: The most frequently identified influenza virus type reported by public health laboratories during week 2 was influenza A, with influenza A (H1N1)pdm09 viruses predominating. The percentage of respiratory specimens testing positive for influenza in clinical laboratories increased.
- Novel Influenza A Virus: One human infection with a novel influenza A virus was reported.
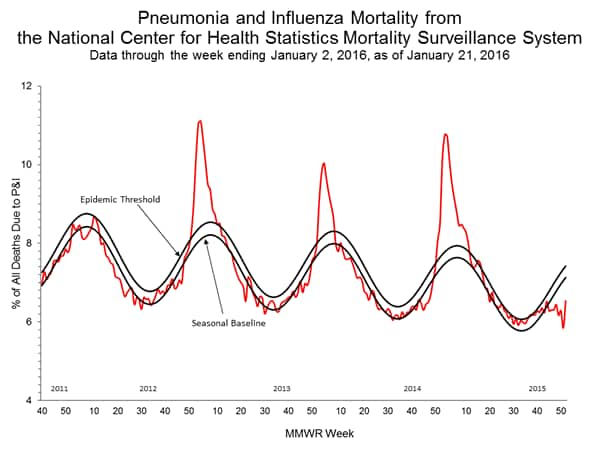
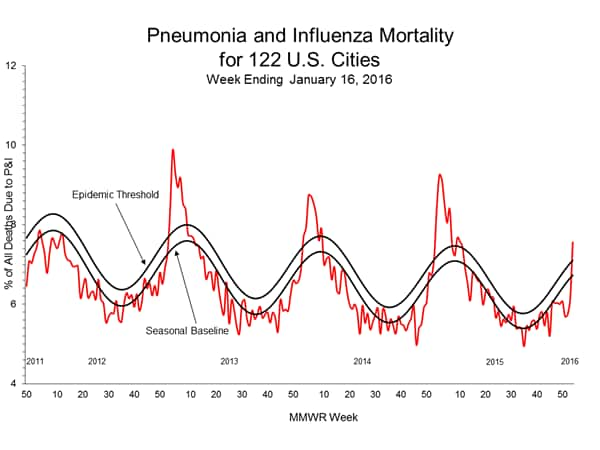
- Pneumonia and Influenza Mortality: The proportion of deaths attributed to pneumonia and influenza (P&I) was below the system-specific epidemic threshold in the NCHS Mortality Surveillance System and above the system-specific epidemic threshold in the 122 Cities Mortality Reporting System.
- Influenza-associated Pediatric Deaths: No influenza-associated pediatric deaths were reported.
- Influenza-associated Hospitalizations: A cumulative rate for the season of 1.8 laboratory-confirmed influenza-associated hospitalizations per 100,000 population was reported.
- Outpatient Illness Surveillance: The proportion of outpatient visits for influenza-like illness (ILI) was 2.1%, which is at the national baseline of 2.1%. Six of 10 regions reported ILI at or above region-specific baseline levels. Puerto Rico experienced high ILI activity; three states experienced moderate ILI activity; New York City and four states experienced low ILI activity; 43 states experienced minimal ILI activity; and the District of Columbia had insufficient data.
- Geographic Spread of Influenza: The geographic spread of influenza in three states was reported as widespread; Puerto Rico and 10 states reported regional activity; Guam and 12 states reported local activity; the U.S. Virgin Islands and 24 states reported sporadic activity; and the District of Columbia and one state reported no influenza activity.
Region and state-specific data are available at http://www.cdc.gov/flu/weekly/nchs.htm.
China: Cause-specific mortality between 1990 and 2013
Sunday, January 24th, 2016In 1990, 16 of 33 provinces had lower respiratory infections or preterm birth complications as the leading causes of YLLs (years of life lost ).
15 provinces had cerebrovascular disease and two (Hong Kong and Macao) had ischaemic heart disease.
By 2013, 27 provinces had cerebrovascular disease as the leading cause, 5 had ischaemic heart disease, and 1 had lung cancer (Hong Kong).
Road injuries have become a top ten cause of death in all provinces in mainland China.
The most common non-communicable diseases, including ischaemic heart disease, stroke, chronic obstructive pulmonary disease, and cancers (liver, stomach, and lung), contributed much more to YLLs in 2013 compared with 1990.
1/23/1556: The infamous Shaanxi, China earthquake kills an estimated 830,000 people.
Saturday, January 23rd, 2016** WHO confirmed that Guyana, Barbados, Ecuador, and Bolivia have joined the ever-growing list of countries affected by Zika virus..
Saturday, January 23rd, 2016Zika virus disease: Questions and answers
Where does Zika virus occur?
Zika virus occurs in tropical areas with large mosquito populations, and is known to circulate in Africa, the Americas, Southern Asia and Western Pacific.
Zika virus was discovered in 1947, but for many years only sporadic human cases were detected in Africa and Southern Asia. In 2007, the first documented outbreak of Zika virus disease occurred in the Pacific. Since 2013, cases and outbreaks of the disease have been reported from the Western Pacific, the Americas and Africa. Given the expansion of environments where mosquitoes can live and breed, facilitated by urbanisation and globalisation, there is potential for major urban epidemics of Zika virus disease to occur globally.
How do people catch Zika virus?
People catch Zika virus by being bitten by an infected Aedes mosquito – the same type of mosquito that spreads dengue, chikungunya and yellow fever.
What are the symptoms of Zika virus disease?
Zika virus usually causes mild illness; with symptoms appearing a few days after a person is bitten by an infected mosquito. Most people with Zika virus disease will get a slight fever and rash. Others may also get conjunctivitis, muscle and joint pain, and feel tired. The symptoms usually finish in 2 to 7 days.
What might be the potential complications of Zika virus?
Because no large outbreaks of Zika virus were recorded before 2007, little is currently known about the complications of the disease.
During the first outbreak of Zika from 2013 – 2014 in French Polynesia, which also coincided with an ongoing outbreak of dengue, national health authorities reported an unusual increase in Guillain-Barré syndrome. Retrospective investigations into this effect are ongoing, including the potential role of Zika virus and other possible factors. A similar observation of increased Guillain-Barré syndrome was also made in 2015 in the context of the first Zika virus outbreak in Brazil.
In 2015, local health authorities in Brazil also observed an increase in babies born with microcephaly at the same time of an outbreak of Zika virus. Health authorities and agencies are now investigating the potential connection between microcephaly and Zika virus, in addition to other possible causes. However more investigation and research is needed before we will be able to better understand any possible link.
Should pregnant women be concerned about Zika?
Health authorities are currently investigating a potential link between Zika virus in pregnant women and microcephaly in their babies. Until more is known, women who are pregnant or planning to become pregnant should take extra care to protect themselves from mosquito bites.
If you are pregnant and suspect that you may have Zika virus disease, consult your doctor for close monitoring during your pregnancy.
What is microcephaly?
Microcephaly is a rare condition where a baby has an abnormally small head. This is due to abnormal brain development of the baby in the womb or during infancy. Babies and children with microcephaly often have challenges with their brain development as they grow older.
Microcephaly can be caused by a variety of environmental and genetic factors such as Downs syndrome; exposure to drugs, alcohol or other toxins in the womb; and rubella infection during pregnancy.
How is Zika virus disease treated?
The symptoms of Zika virus disease can be treated with common pain and fever medicines, rest and plenty of water. If symptoms worsen, people should seek medical advice. There is currently no cure or vaccine for the disease itself.
How is Zika virus disease diagnosed?
For most people diagnosed with Zika virus disease, diagnosis is based on their symptoms and recent history (e.g. mosquito bites, or travel to an area where Zika virus is known to be present). A laboratory can confirm the diagnosis by blood tests.
What can I do to protect myself?
The best protection from Zika virus is preventing mosquito bites. Preventing mosquito bites will protect people from Zika virus, as well as other diseases that are transmitted by mosquitoes such as dengue, chikungunya and yellow fever.
This can be done by using insect repellent; wearing clothes (preferably light-coloured) that cover as much of the body as possible; using physical barriers such as screens, closed doors and windows; and sleeping under mosquito nets. It is also important to empty, clean or cover containers that can hold water such as buckets, flower pots or tyres, so that places where mosquitoes can breed are removed.
Should I avoid travelling to areas where Zika virus is occurring?
Travellers should stay informed about Zika virus and other mosquito-borne diseases and consult their local health or travel authorities if they are concerned.
To protect against Zika virus and other mosquito-borne diseases, everyone should avoid being bitten by mosquitoes by taking the measures described above. Women who are pregnant or planning to become pregnant should follow this advice, and may also consult their local health authorities if travelling to an area with an ongoing Zika virus outbreak.
Based on available evidence, WHO is not recommending any travel or trade restrictions related to Zika virus disease. As a precautionary measure, some national governments may make public health and travel recommendations to their own populations, based on their assessments of the available evidence and local risk factors.
What is WHO doing?
To help countries prepare for and respond to Zika, WHO is working with ministries of health to improve laboratory capacity to detect the virus, providing recommendations for clinical care and follow-up of infected patients (in collaboration with national professional associations and experts), and encouraging monitoring and reporting on the virus’s spread and the emergence of complications.
WHO is also coordinating with countries that have reported outbreaks of Zika virus and other partners to investigate the potential relationships between Zika and microcephaly and other issues.
CDC adds new destinations to the Zika virus travel alerts: Barbados, Bolivia, Ecuador, Guadeloupe, Saint Martin, Guyana, Cape Verde, and Samoa.
Saturday, January 23rd, 2016CDC adds countries to interim travel guidance related to Zika virus
As more information becomes available, CDC travel alerts will be updated. Travelers to areas where cases of Zika virus infection have been recently confirmed are at risk of being infected with the Zika virus. Travelers to these areas may also be at risk of being infected with dengue or chikungunya viruses. Mosquitoes that spread Zika, chikungunya, and dengue are aggressive daytime biters, prefer to bite people, and live indoors and outdoors near people. There is no vaccine or medicine available for Zika virus. The best way to avoid Zika virus infection is to prevent mosquito bites.
Some travelers to areas with ongoing Zika virus transmission will become infected while traveling but will not become sick until they return home. Symptoms include fever, rash, joint pain, and red eyes. Other commonly reported symptoms include muscle pain, headache, and pain behind the eyes. The illness is usually mild with symptoms lasting from several days to a week. Severe disease requiring hospitalization is uncommon and case fatality is low. Travelers to these areas should monitor for symptoms or illness upon return. If they become ill, they should tell their healthcare professional where they have traveled and when.
Until more is known, and out of an abundance of caution, CDC continues to recommend that pregnant women and women trying to become pregnant take the following precautions:
- Pregnant women in any trimester should consider postponing travel to the areas where Zika virus transmission is ongoing. Pregnant women who must travel to one of these areas should talk to their doctor or other healthcare professional first and strictly follow steps to avoid mosquito bites during the trip.
- Women trying to become pregnant should consult with their healthcare professional before traveling to these areas and strictly follow steps to prevent mosquito bites during the trip.
Guillain-Barré syndrome (GBS) has been reported in patients with probable Zika virus infection in French Polynesia and Brazil. Research efforts will also examine the link between Zika and GBS.