Archive for January, 2016
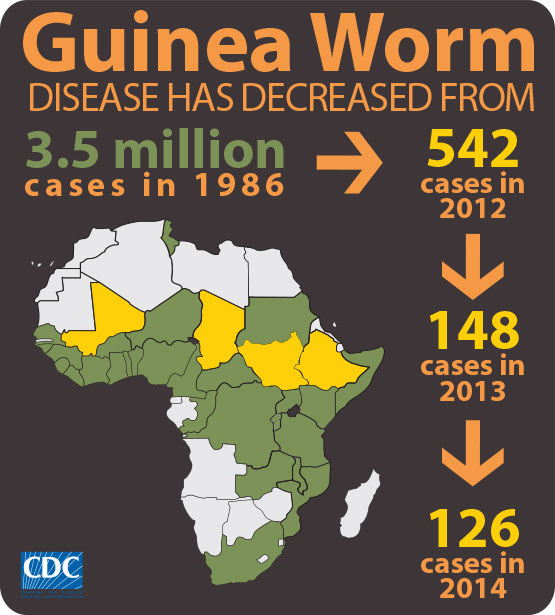
** Guinea worm disease on the way out!
Tuesday, January 19th, 2016** Only 22 cases of Guinea worm disease were reported in 2015,
** 126 cases reported in 2014.
** When the campaign began, there were an estimated 3.5 million cases of Guinea worm infestation
** The cases were spread across 20 villages in four countries (Chad, Ethiopia, Mali, and South Sudan)
** Guinea worms have been found in hundreds of dogs in Chad, raising the danger that they have found a new host.
** Guinea worm and polio are the two diseases now closest to being eliminated.
** There were only 70 cases of polio paralysis in the world last year, all in Pakistan and Afghanistan.
Causal Agent:
Dracunculiasis (guinea worm disease) is caused by the nematode (roundworm) Dracunculus medinensis.
Life Cycle:
Humans become infected by drinking unfiltered water containing copepods (small crustaceans) which are infected with larvae of D. medinensis ![]() . Following ingestion, the copepods die and release the larvae, which penetrate the host stomach and intestinal wall and enter the abdominal cavity and retroperitoneal space
. Following ingestion, the copepods die and release the larvae, which penetrate the host stomach and intestinal wall and enter the abdominal cavity and retroperitoneal space ![]() . After maturation into adults and copulation, the male worms die and the females (length: 70 to 120 cm) migrate in the subcutaneous tissues towards the skin surface
. After maturation into adults and copulation, the male worms die and the females (length: 70 to 120 cm) migrate in the subcutaneous tissues towards the skin surface ![]() . Approximately one year after infection, the female worm induces a blister on the skin, generally on the distal lower extremity, which ruptures. When this lesion comes into contact with water, a contact that the patient seeks to relieve the local discomfort, the female worm emerges and releases larvae
. Approximately one year after infection, the female worm induces a blister on the skin, generally on the distal lower extremity, which ruptures. When this lesion comes into contact with water, a contact that the patient seeks to relieve the local discomfort, the female worm emerges and releases larvae ![]() . The larvae are ingested by a copepod
. The larvae are ingested by a copepod ![]() and after two weeks (and two molts) have developed into infective larvae
and after two weeks (and two molts) have developed into infective larvae ![]() . Ingestion of the copepods closes the cycle
. Ingestion of the copepods closes the cycle ![]() .
.
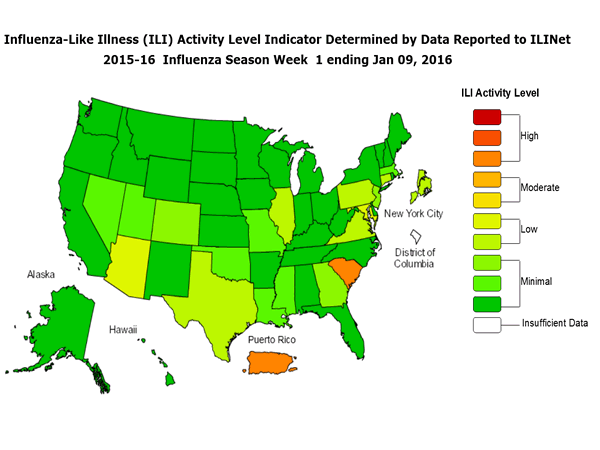
CDC: 2015-2016 Influenza Season Week 1 ending January 9, 2016
Monday, January 18th, 2016Background:
The Centers for Disease Control and Prevention’s (CDC) Influenza Division collects, compiles, and analyzes information on influenza activity year-round in the United States and produces FluView, a weekly influenza surveillance report, and FluView Interactive. The U.S. influenza surveillance system provides information in five categories collected from nine data sources. This is the first report of the 2015-2016 influenza season, which began on October 4, 2015.
The five categories and nine data components of CDC influenza surveillance are:
- Viral Surveillance:U.S. World Health Organization (WHO) collaborating laboratories, the National Respiratory and Enteric Virus Surveillance System (NREVSS), and human infection with novel influenza A virus case reporting;
- Mortality:National Center for Health Statistics (NCHS) Mortality Surveillance System, 122 Cities Mortality Reporting System and influenza-associated pediatric deaths;
- Hospitalizations:Influenza Hospitalization Network (FluSurv-NET) including the Emerging Infections Program (EIP) and three additional states;
- Outpatient Illness Surveillance:U.S. Outpatient Influenza-like Illness Surveillance Network (ILINet);
- Geographic Spread of Influenza:State and territorial epidemiologists’ reports.
An overview of the CDC influenza surveillance system, including methodology and detailed descriptions of each data component, is available at: http://www.cdc.gov/flu/weekly/overview.htm.
–>
Synopsis:
During week 1 (January 3-9, 2016), laboratory data indicated that influenza activity increased slightly in the United States.
- Viral Surveillance: The most frequently identified influenza virus type reported by public health laboratories during week 1 was influenza A, with influenza A (H1N1)pdm09 viruses predominating. The percentage of respiratory specimens testing positive for influenza in clinical laboratories was low.
<!–
- Novel Influenza A Virus: One human infection with a novel influenza A virus was reported.
–>
- Pneumonia and Influenza Mortality: The proportion of deaths attributed to pneumonia and influenza (P&I) was below their system-specific epidemic threshold in both the NCHS Mortality Surveillance System and the 122 Cities Mortality Reporting System.
- Influenza-associated Pediatric Deaths: One influenza-associated pediatric death was reported.
- Influenza-associated Hospitalizations: A cumulative rate for the season of 1.5 laboratory-confirmed influenza-associated hospitalizations per 100,000 population was reported.
- Outpatient Illness Surveillance: The proportion of outpatient visits for influenza-like illness (ILI) was 2.0%, which is below the national baseline of 2.1%. Four of 10 regions reported ILI at or above region-specific baseline levels. Puerto Rico and one state experienced high ILI activity; New York City and seven states experienced low ILI activity; 42 states experienced minimal ILI activity; and the District of Columbia had insufficient data.
- Geographic Spread of Influenza: The geographic spread of influenza in Guam, Puerto Rico, and nine states were reported as regional; 11 states reported local activity; the U.S. Virgin Islands and 28 states reported sporadic activity; and the District of Columbia and two states reported no influenza activity.
Honduran bus crash: “…In this case, the students’ humanitarian mission ended in tragedy. The bus accident killed 3 students and left students and staff at Columbia in shock. It also highlighted the difficult issues colleges and universities face when students decide to volunteer in sometimes dangerous parts of the world….”
Monday, January 18th, 2016
“……The Columbia students were on a trip organized by Global Brigades, a student-run nonprofit dedicated to bringing health care and economic development programs to communities in Latin America and West Africa……”

HAWAII DEPARTMENT OF HEALTH RECEIVES CONFIRMATION OF ZIKA INFECTION IN BABY BORN WITH MICROCEPHALY
Sunday, January 17th, 2016The Hawaii State Department of Health (DOH) has received laboratory confirmation from the U.S. Centers for Disease Control and Prevention (CDC) of a past Zika virus infection in a baby recently born with microcephaly in a hospital on Oahu. The mother likely had Zika infection when she was residing in Brazil in May 2015 and her newborn acquired the infection in the womb. Neither the baby nor the mother are infectious, and there was never a risk of transmission in Hawaii.
“We are saddened by the events that have affected this mother and her newborn,” said DOH State Epidemiologist Dr. Sarah Park. “This case further emphasizes the importance of the CDC travel recommendations released today. Mosquitos can carry serious diseases, as we know too well with our current dengue outbreak and it is imperative that we all Fight the Bite by reducing mosquito breeding areas, avoiding places with mosquitos, and applying repellant as needed.”
To date, there have been no cases of Zika virus acquired in Hawaii. Since 2014, the department has identified six persons in the state who acquired their infection in another country. Physicians are required to report all suspected cases of Zika virus and more than 75 other reportable diseases in the state. Physician reporting is crucial to conducting an effective disease surveillance program in Hawaii.
“In this situation, an astute Hawaii physician recognized the possible role of Zika virus infection, immediately notified the Department of Health, and worked with us to confirm the suspected diagnosis,” said Dr. Park. “We rely on our exceptional medical community to be our eyes and ears in the field to control and prevent the spread of illness in Hawaii.”
The department sent a Medical Advisory to physicians statewide today as a reminder that while Zika virus is not endemic in the U.S., it can be acquired in a number of countries and travel history should always be considered.
Zika virus is spread to people through mosquito bites. The most common symptoms of Zika virus disease are fever, rash, joint pain, and conjunctivitis (red eyes). The illness is usually mild with symptoms lasting from several days to a week. Severe disease requiring hospitalization is uncommon. There is no vaccine to prevent or medicine to treat Zika.
In the Syrian city of Deir al-Zor: 200,000 residents face a severe food shortage and sharply deteriorating conditions.
Sunday, January 17th, 2016Burkina Faso : 126 hostages freed, but 23 killed in Hotel Splendid siege
Saturday, January 16th, 2016
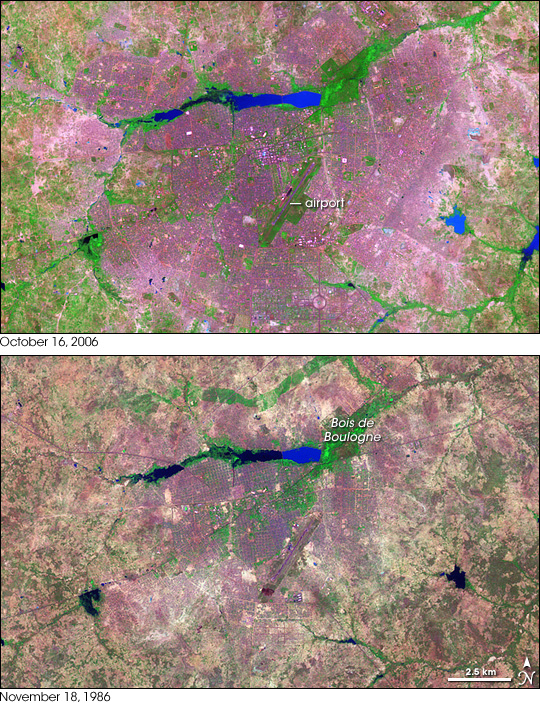
NASA: In western Africa, just south of the Sahara Desert, lies the landlocked nation of Burkina Faso. Despite the limited natural resources in this arid savannah, the nation experienced a 200 percent increase in urban population between 1975 and 2000. Much of that growth occurred in the capital city of Ouagadougou, where unplanned settlements sprang up along the city’s perimeter. Between 1960 and 1993, Ouagadougou experienced a 14-fold increase in area.
Over the years, NASA’s Landsat satellites have observed the increase in Ouagadougou’s extent. The Landsat 7 satellite captured the top image on October 16, 2006, and the Landsat 5 satellite acquired the bottom image on November 18, 1986. In these false-color images, vegetation appears bright green, bare or sparsely vegetated ground ranges in color from beige to gray-green, and water ranges in color from navy to electric blue. Paved surfaces and buildings appear pink-purple.
The 2006 image shows how urbanization radiated out from the city center, filling nearly the entire frame. Urbanization has increased especially in the east and south; in the 1986 image, random shapes of green and brown fill the area; in the 2006 image, that area is predominantly pinkish purple. Likewise, a crooked line of vegetation that is visible north of Bois de Boulogne in 1986 has all but disappeared in 2006.
In both images, the Ouagadougou airport appears as a conspicuous diagonal line near the center of the image. In 1986, the airport lies fairly close to the city’s outskirts. In 2006, continued urbanization has surrounded the airport with cityscape. Southwest of the airport, the beginnings of urbanization appear in 1986, and that urbanization is more pronounced in 2006.
Lakes and rivers near the top and right edges of the image show different colors between 1986 and 2006; the color change likely results from differences in sediment or organic matter suspended in the water.
In 2008, the United Nations Environment Programme (UNEP) published Africa: Atlas of Our Changing Environment highlighting changes detected by remote sensing, and providing overviews of each nation’s progress toward environmental sustainability in the late twentieth and early twenty-first century. UNEP found that, in the 1980s, Ouagadougou’s growth resulted predominantly from rural-to-urban migration. After that time, the population increased primarily from natural growth—birth rates exceeding death rates. The growth led to an explosion of unplanned settlements. Unplanned settlements may conflict with sustainable development goals, and they make it harder for the government to provide basic services, such as drinking water.
Despite growing urbanization, however, UNEP found that Burkina Faso made progress in some key areas of environmental sustainability. Protected areas increased slightly from 1990 to 2005, and per capita carbon dioxide emissions dropped slightly over roughly the same period. Meanwhile, access to better sources of drinking water and sanitation increased from 1990 to 2004, and the proportion of urban dwellers living in slums decreased slightly from 1990 to 2001. Nevertheless, water scarcity, desertification, and deforestation all threatened the country’s future health.
- References
- United Nations Environment Programme. (2008). Africa: Atlas of Our Changing Environment. Division of Early Warning and Assessment, United Nations Environment Programme, Nairobi, Kenya.
CDC HEALTH ADVISORY on Zika virus, travel, and pregnant women
Saturday, January 16th, 2016Recognizing, Managing, and Reporting Zika Virus Infections in Travelers Returning from Central America, South America, the Caribbean, and Mexico
This is an official
CDC HEALTH ADVISORY
Distributed via the CDC Health Alert Network
Friday, January 15, 2016, 19:45 EST (7:45 PM EST)
CDCHAN-00385
Summary
In May 2015, the World Health Organization reported the first local transmission of Zika virus in the Western Hemisphere, with autochthonous (locally acquired) cases identified in Brazil. As of January 15, 2016, local transmission had been identified in at least 14 countries or territories in the Americas, including Puerto Rico (See Pan American Health Organization [PAHO] link below for countries and territories in the Americas with Zika virus transmission). Further spread to other countries in the region is likely.
Local transmission of Zika virus has not been documented in the continental United States. However, Zika virus infections have been reported in travelers returning to the United States. With the recent outbreaks in the Americas, the number of Zika virus disease cases among travelers visiting or returning to the United States likely will increase. These imported cases may result in local spread of the virus in some areas of the continental United States, meaning these imported cases may result in human-to-mosquito-to-human spread of the virus.
Zika virus infection should be considered in patients with acute onset of fever, maculopapular rash, arthralgia or conjunctivitis, who traveled to areas with ongoing transmission in the two weeks prior to illness onset. Clinical disease usually is mild. However, during the current outbreak, Zika virus infections have been confirmed in several infants with microcephaly and in fetal losses in women infected during pregnancy. We do not yet understand the full spectrum of outcomes that might be associated with infection during pregnancy, nor the factors that might increase risk to the fetus. Additional studies are planned to learn more about the risks of Zika virus infection during pregnancy.
Healthcare providers are encouraged to report suspected Zika virus disease cases to their state health department to facilitate diagnosis and to mitigate the risk of local transmission. State health departments are requested to report laboratory-confirmed cases to CDC. CDC is working with states to expand Zika virus laboratory testing capacity, using existing RT-PCR protocols.
This CDC Health Advisory includes information and recommendations about Zika virus clinical disease, diagnosis, and prevention, and provides travel guidance for pregnant women and women who are trying to become pregnant.
Until more is known and out of an abundance of caution, pregnant women should consider postponing travel to any area where Zika virus transmission is ongoing.
Pregnant women who do travel to these areas should talk to their doctors or other healthcare providers first and strictly follow steps to avoid mosquito bites during the trip. Women trying to become pregnant should consult with their healthcare providers before traveling to these areas and strictly follow steps to avoid mosquito bites during the trip.
Background
Zika virus is a mosquito-borne flavivirus transmitted primarily by Aedes aegypti. Aedes albopictus mosquitoes might also transmit the virus. Outbreaks of Zika virus disease have been reported previously in Africa, Asia, and islands in the Pacific.
Clinical Disease
About one in five people infected with Zika virus become symptomatic. Characteristic clinical findings include acute onset of fever, maculopapular rash, arthralgia, or conjunctivitis. Clinical illness usually is mild with symptoms lasting for several days to a week. Severe disease requiring hospitalization is uncommon and fatalities are rare. During the current outbreak in Brazil, Zika virus RNA has been identified in tissues from several infants with microcephaly and from fetal losses in women infected during pregnancy. The Brazil Ministry of Health has reported a marked increase in the number of babies born with microcephaly. However, it is not known how many of the microcephaly cases are associated with Zika virus infection and what factors increase risk to the fetus. Guillain-Barré syndrome also has been reported in patients following suspected Zika virus infection.
Diagnosis
Zika virus infection should be considered in patients with acute onset of fever, maculopapular rash, arthralgia, or conjunctivitis who recently returned from affected areas. To confirm evidence of Zika virus infection, RT-PCR should be performed on serum specimens collected within the first week of illness. Immunoglobulin M and neutralizing antibody testing should be performed on specimens collected ≥4 days after onset of illness. Zika virus IgM antibody assays can be positive due to antibodies against related flaviviruses (e.g., dengue and yellow fever viruses). Virus-specific neutralization testing provides added specificity but might not discriminate between cross-reacting antibodies in people who have been previously infected with or vaccinated against a related flavivirus.
There is no commercially available test for Zika virus. Zika virus testing is performed at the CDC Arbovirus Diagnostic Laboratory and a few state health departments. CDC is working to expand laboratory diagnostic testing in states, using existing RT-PCR protocols. Healthcare providers should contact their state or local health department to facilitate testing.
Treatment
No specific antiviral treatment is available for Zika virus disease. Treatment is generally supportive and can include rest, fluids, and use of analgesics and antipyretics. Because of similar geographic distribution and symptoms, patients with suspected Zika virus infections also should be evaluated and managed for possible dengue or chikungunya virus infection. Aspirin and other non-steroidal anti-inflammatory drugs (NSAIDs) should be avoided until dengue can be ruled out to reduce the risk of hemorrhage. In particular, pregnant women who have a fever should be treated with acetaminophen. People infected with Zika, chikungunya, or dengue virus should be protected from further mosquito exposure during the first few days of illness to reduce the risk of local transmission.
Prevention
No vaccine or preventive drug is available. The best way to prevent Zika virus infection is to:
- Avoid mosquito bites.
- Use air conditioning or window and door screens when indoors.
- Wear long sleeves and pants, and use insect repellents when outdoors. Most repellents, including DEET, can be used on children older than two months. Pregnant and lactating women can use all Environmental Protection Agency (EPA)-registered insect repellents, including DEET, according to the product label.
Recommendations for Health Care Providers and Public Health Practitioners
- Zika virus infection should be considered in patients with acute fever, rash, arthralgia, or conjunctivitis, who traveled to areas with ongoing transmission in the two weeks prior to onset of illness.
- All travelers should take steps to avoid mosquito bites to prevent Zika virus infection and other mosquito-borne diseases.
- Until more is known and out of an abundance of caution, pregnant women should consider postponing travel to any area where Zika virus transmission is ongoing. Pregnant women who do travel to one of these areas should talk to their doctors or other healthcare providers first and strictly follow steps to avoid mosquito bites during the trip. Women trying to become pregnant should consult with their healthcare providers before traveling to these areas and strictly follow steps to avoid mosquito bites during the trip.
- Fetuses and infants of women infected with Zika virus during pregnancy should be evaluated for possible congenital infection and neurologic abnormalities.
- Healthcare providers are encouraged to report suspected Zika virus disease cases to their state or local health department to facilitate diagnosis and to mitigate the risk of local transmission.
- Health departments should perform surveillance for Zika virus disease in returning travelers and be aware of the risk of possible local transmission in areas where Aedes species mosquitoes are active.
- State health departments are requested to report laboratory-confirmed Zika virus infections to CDC.
For More Information
- General information about Zika virus and disease: http://www.cdc.gov/zika/
- Zika virus information for clinicians: http://www.cdc.gov/zika/hc-providers/index.html
- Protection against mosquitoes: http://wwwnc.cdc.gov/travel/yellowbook/2016/the-pre-travel-consultation/protection-against-mosquitoes-ticks-other-arthropods
- Travel notices related to Zika virus: http://wwwnc.cdc.gov/travel/notices
- Information about Zika virus for travelers and travel health providers: http://wwwnc.cdc.gov/travel/yellowbook/2016/infectious-diseases-related-to-travel/zika
- Pan American Health Organization (PAHO): http://www.cdc.gov/ncbddd/birthdefects/microcephaly.html
- Approximate distribution of Aedes aegypti and Ae. albopictus mosquitoes in the United States: http://www.cdc.gov/chikungunya/resources/vector-control.html
The Centers for Disease Control and Prevention (CDC) protects people’s health and safety by preventing and controlling diseases and injuries; enhances health decisions by providing credible information on critical health issues; and promotes healthy living through strong partnerships with local, national and international organizations.